Body fluids are liquids found inside the body of living organisms. They play a very important role in keeping the body alive and working properly. In animals, including humans, body fluids help in transporting nutrients, oxygen, hormones, and waste materials. They also help maintain temperature and protect the body from infections.
Main Types of Body Fluids
In humans and other higher animals, the main body fluids are:
- Blood
- Lymph
- Tissue Fluid (Interstitial Fluid)
Blood
Blood is the most important body fluid. It flows through blood vessels and carries essential substances.
- Components of blood:
- Plasma – A yellowish liquid that makes up about 55% of blood. It contains water, salts, proteins, hormones, and waste materials.
- Red Blood Cells (RBCs) – Carry oxygen from the lungs to body cells and bring back carbon dioxide to the lungs.
- White Blood Cells (WBCs) – Defend the body against germs and infections.
- Platelets – Help in clotting of blood when there is an injury.
- Functions of blood:
- Transports oxygen, nutrients, and hormones.
- Removes waste materials like carbon dioxide and urea.
- Maintains body temperature.
- Protects the body from infections.
Lymph
Lymph is a clear, colorless fluid that flows in lymphatic vessels.
-
- Components: Mostly water, proteins, and white blood cells.
- Functions:
- Returns excess tissue fluid to the blood.
- Helps in fighting infections.
- Transports fats and fat-soluble vitamins from the digestive system to the blood.
Tissue Fluid (Interstitial Fluid)
This fluid surrounds the cells in tissues. It comes from blood plasma and allows the exchange of nutrients and waste products between blood and cells.
- Functions:
- Provides oxygen and nutrients to cells.
- Removes carbon dioxide and other waste from cells.
Importance of Body Fluids
Body fluids are essential for:
- Carrying food, oxygen, and hormones to cells.
- Removing waste products from the body.
- Maintaining the right temperature for proper functioning.
- Protecting the body from diseases through immune cells.
- Helping in chemical reactions by providing a watery environment.
Disorders Related to Body Fluids
- Dehydration – Lack of water in the body fluids, leading to weakness.
- Anemia – Low red blood cells or hemoglobin, reducing oxygen transport.
- Infections – Germs in blood or lymph can cause diseases.
Circulation
Circulatory system functionally connects body cells with the organ of exchange. It also functions in homeostasis, enabling other organ system to regulate the chemical and physical properties of the cellular environment.
Types of Circulation
Intra-circular
Example: Cyclosis (cytoplasmic streaming) occurs in all eukaryotic cells.
Extra-circular
Extra-organismic
- Sponges: Water canal system
- Cnidarians: Gastrovascular circulation
- Echinoderms: Water vascular system
Intra-organismic
- Platyhelminthes: Parenchymal
- Aschleminthes: Pseudocoelomic
- Arthropods: Haemocoelomic
- Annelids to chordates: Blood Vascular System (BVS)
Blood Vascular System (BVS)
Blood Vascular System is of 2 types:
| Open Blood Vascular System | Closed Blood Vascular System |
|
|
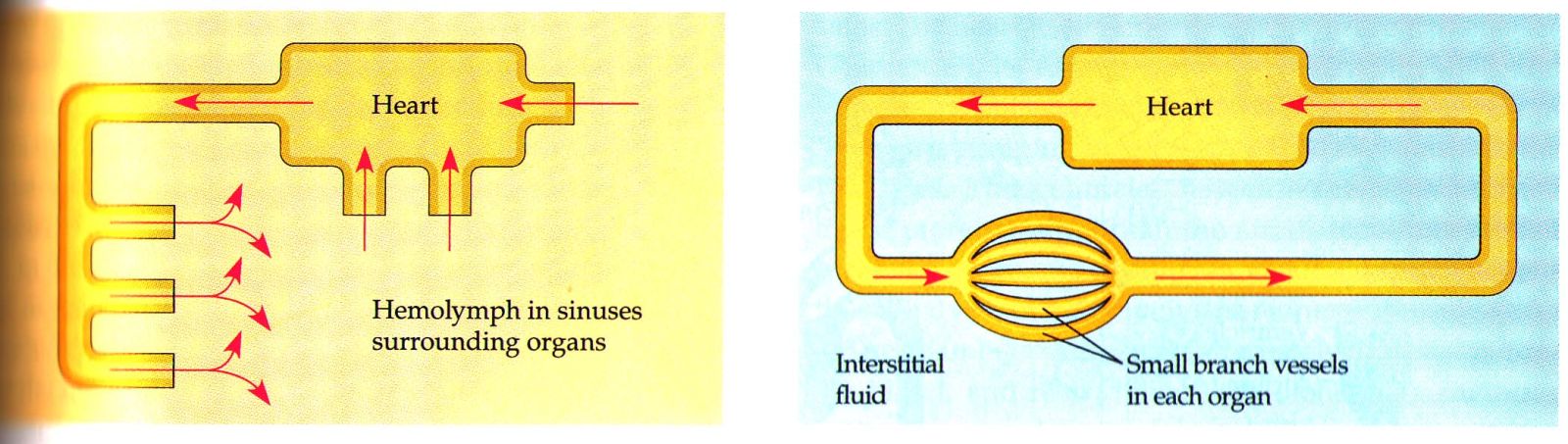
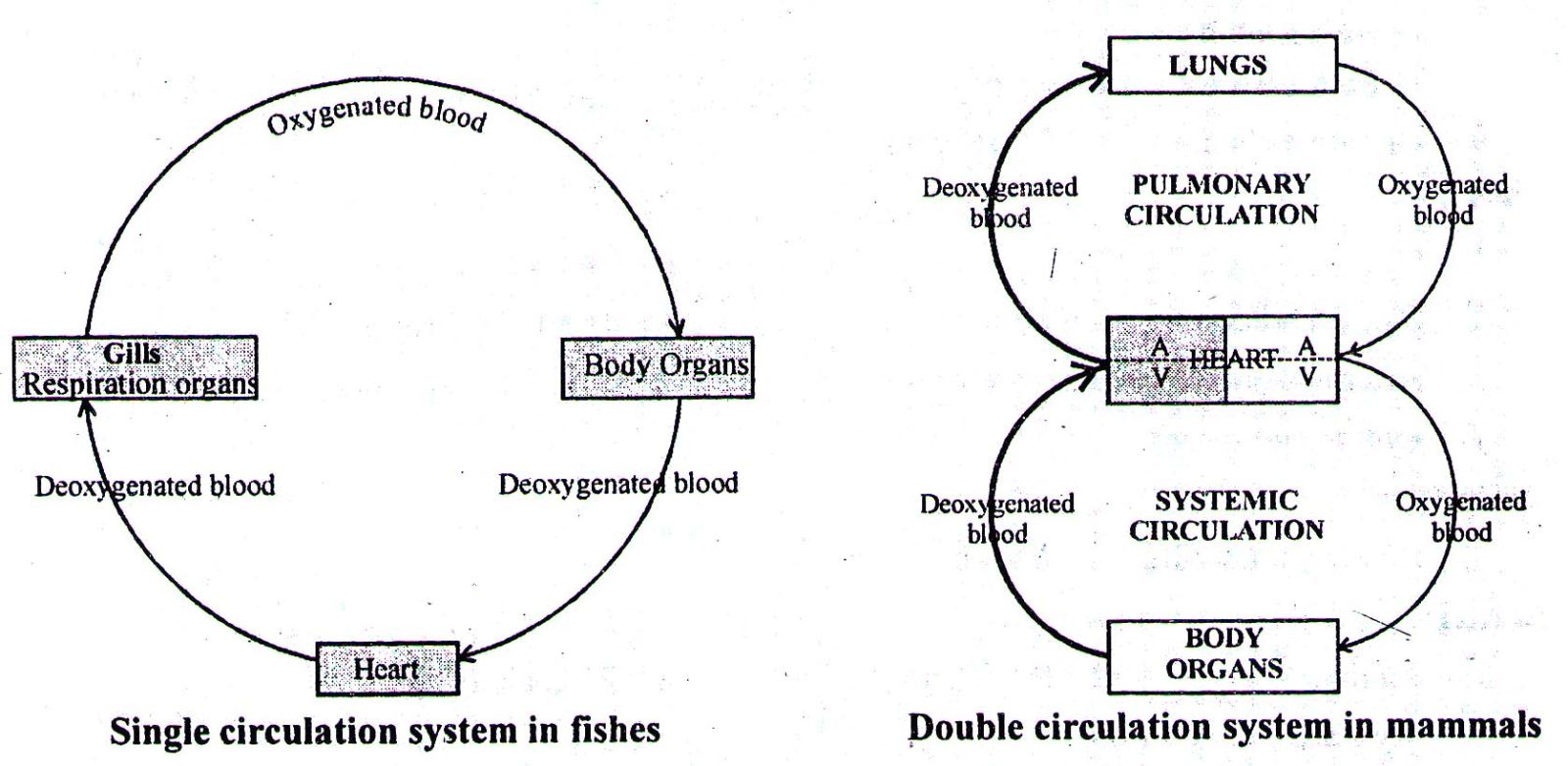
Types of Closed Blood Vascular System
| Single Circulation System | Double Circulation System |
|
|
Comparative Morphology of Heart in Different Vertebrates
- Fishes: 2-chambered heart (1 Atrium + 1 Ventricle). Heart is Venous heart.
- Amphibians: 3-chambered heart (2A + 1V). Due to single ventricle, blood in frog is mixed in this chamber.
- Reptiles: Generally incompletely 4-chambered heart. However, in Crocodile and Alligator the heart is completely 4-chambered (2A + 2V).
- Birds and Mammals: Always 4-chambered heart (2A + 2V)
Blood and Lymph
Blood is a red coloured, thick and slightly alkaline pH (7.4 – 7.6) fluid, which keeps circulating through the blood vessels in our body. Blood is a fluid connective tissue made up of plasma and blood cells.
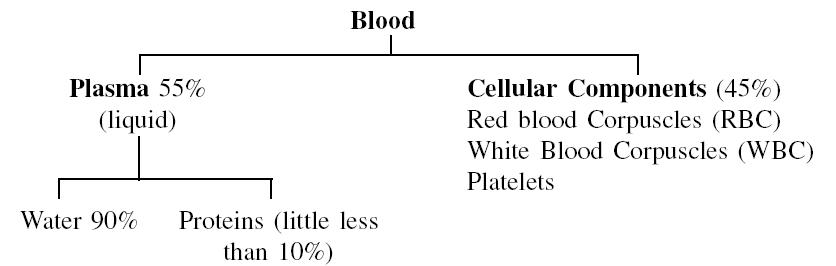
A. Plasma (55%)
It is a pale yellow liquid consisting of blood proteins like albumin, globulin and fibrinogen.
Functions of Plasma:
- Transport of products of digestion from small intestine to various tissues
- Transport of waste products from tissues to excretory organs
- Transport of hormones from endocrine glands to target organs
- Maintenance of temperature by distribution of heat all over the body
- Provide factors for clotting of blood (Fibrinogen)
- Retention of fluids in blood (through plasma proteins)
- Maintenance of acid-base equilibrium of blood
- Provides body immunity through antibodies (Immunoglobulins) which are made by a type of WBC's and then released into the plasma
- Albumin as major blood plasma protein helps in maintaining blood osmotic pressure
B. Blood Cells (45%)
The cells of blood are Red Blood Corpuscles (RBC), White Blood Corpuscles (WBC) and cell fragments the Platelets. Blood cells are formed in the bone marrow. Their formation is termed haemopoiesis.
Cellular Components of Blood
| Component | Origin of cells/mm³ | Number | Function |
| Erythrocytes (Red Blood Corpuscle) | Bone marrow | 5,000,000 |
|
| Leucocytes (White Blood Corpuscles) | Bone marrow | 4,000-8,000 | |
| (a) Granulocytes (72% of total white blood cell count) | |||
| neutrophils (70%) | Bone marrow | 4900-105 |
|
| eosinophils (1.5%) | 35 |
|
|
| basophils (0.5%) | |||
| (b) Agranulocytes (28%) | |||
| monocytes (4%) | Bone marrow | 280 |
|
| lymphocytes (24%) | Bone marrow, lymphoid tissue, spleen | 1680 |
|
| Platelets | Bone marrow | 250,000 | Initiate blood-clotting |
*Numbers of blood cells are given in per/mm³.
Blood Clotting
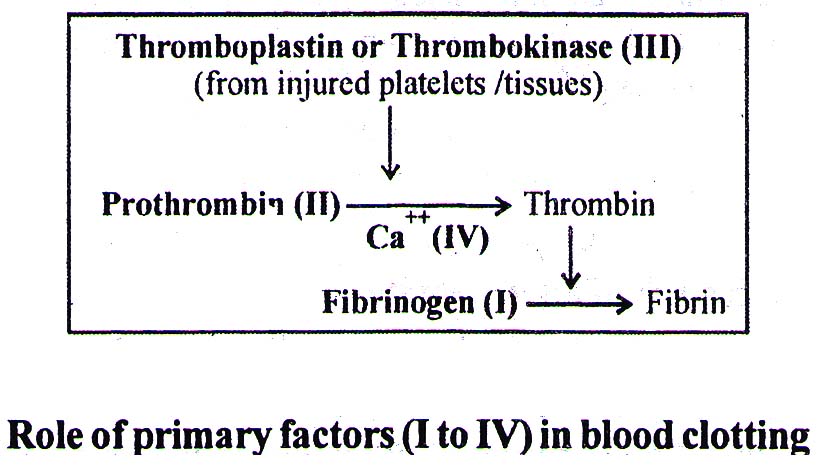
According to Macferlane hypothesis there are 13-factors responsible for blood clotting (or coagulation). The 4-factors are primary and 9-factors are accessory for this process.
Primary Factors
- Fibrinogen
- Prothrombin
- Thromboplastin (Thrombokinase)
- Calcium ions
The thromboplastin is released from injured platelets or injured tissue. This converts prothrombin into thrombin in the presence of calcium ions. The thrombin converts fibrinogen into fibrin, the latter forms the clot. The blood cells are entangled in the network of fibrin. A straw-coloured fluid, separated from clot, is called Serum. As the Serum does not have fibrinogen, it can not clot.
Some Important Accessory Factors
- viii) Anti-haemophilic globulin (AHG): The absence of this factor delays blood clotting causing Haemophilia - A.
- ix) Plasma thromboplastin co-factor (PTC): The deficiency of this factor causes Haemophilia – B. The IX factor is also known as Christmas factor, and Haemophilia B is known as 'Christmas disease'.
- x) Stuart factor: It helps in the conversion of prothrombin into thrombin.
- xi) Plasma thromboplastin antecedent (PTA): The deficiency of this causes a rare type of bleeder-disease, called Haemophilia – C.
Anticoagulants
- Inside body: Heparin is a natural anticoagulant present in the blood. It prevents conversion of prothrombin into thrombin and does not allow blood coagulation inside blood vessels.
- Outside body: Sodium citrate, sodium oxalate, double oxalate and EDTA (ethylene diamine tetra acetic acid) and the other chelating agents bind with free calcium and prevent the conversion of prothrombin into thrombin. Dicumarol and Warfarin inhibit the action of vitamin K (anti prothrombin function) and thus prevent blood clotting.
Blood Groups
The blood may chemically be identified as belonging to any one of the four main group-A, B, AB, and O. Blood types remain constant throughout lifetime as they are hereditary. These blood groups are due to the presence of special glycoproteins present on the membrane of RBCs termed antigens. Antigens present could be A, B both A and B or no Antigen may be present at all. Blood plasma, on the other hand, contains antibodies a, b, or both a and b, or neither of the two. Antigen A reacts with antibody B and antigen B with antibody A causing clumping of blood.
| Blood Group | Antigen | Antibody |
| A | A | b |
| B | B | a |
| AB | A, B | – |
| O | – | a, b |
- Blood group of O type can be given to all groups. It is thus the Universal Donor. This is because there are no antigens in the blood of Group O.
- Blood group AB can receive blood from all other groups and is thus called Universal Recipient. No Antibodies in the blood of Group AB, so no reaction with antigens of other blood groups.
Rh Factor
- Presence or absence of another blood protein in addition of ABO antigens makes a person Rh+ or Rh–.
- Rh factor in expectant mothers can sometimes cause problems. The blood of an Rh+ embryo whose mother is Rh– is in danger of severe clumping (Erythroblastosis foetalis).
- Antibodies are produced in the mother against the Rh+ blood cells of the embryo. Whenever there is even the slightest mixing of foetal blood with mothers blood.
Lymph
Exchange of nutrients, gases, etc., between the blood and the cells always occur through this fluid. An elaborate network of vessels called the lymphatic system collects this fluid and drains it back to the major veins. The fluid present in the lymphatic system is called the lymph.
- It is mostly described as Blood minus RBCs. It can also be represented as plasma plus WBCs.
- In lymph, the number of WBCs is lesser but the percentage of lymphocytes is greater than blood.
- In comparison to blood plasma, the proteins in lymph are fewer.
- Like plasma the lymph also contains fibrinogen and hence can clot.
Human Heart
- Heart, the mesodermally derived organ, is situated in the thoracic cavity, in between the two lungs, slightly tilted to the left.
- It is 10 – 12 cm in size, and is present in the mediastinum (space between two lungs).
- It Weighs 250g in males and 225g in females.
- The heart is covered by a transparent serous membrane, the pericardium (the parietal mesoderm/peritoneum). The pericardial fluid between heart and the pericardium keeps the heart moist, protects it from friction and mechanical injury.
- The wall of the heart has 3-coatings, Epicardium (outer), Myocardium (Middle) and Endocardium (inner). The myocardium contains cardiac muscles.
- The atria and ventricles are divided by Coronary Sulcus.
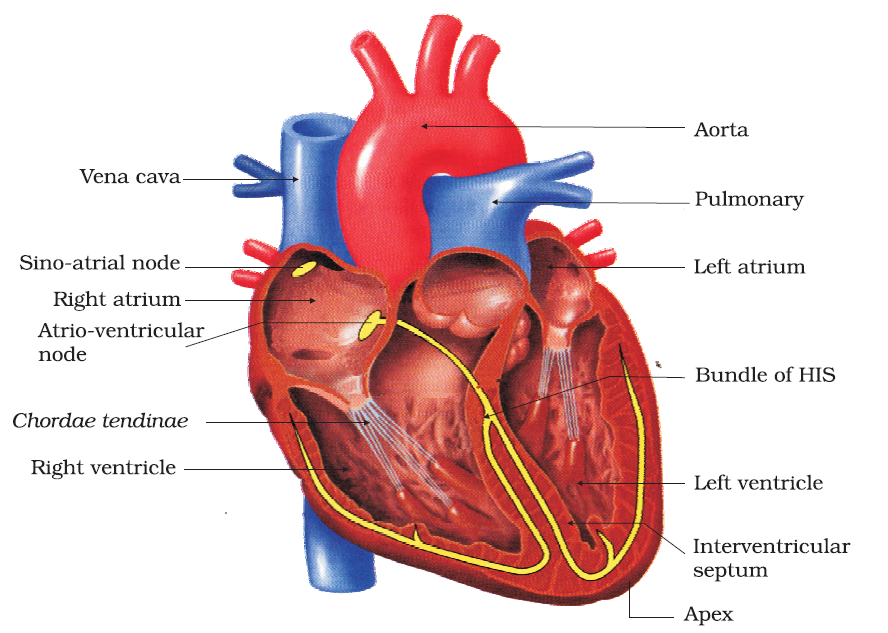
Heart Chambers and Valves
- The atrium and the ventricle of the same side are also separated by a thick fibrous tissue called the atrio-ventricular septum. However, each of these septa is provided with an opening through which the two chambers of the same side reconnected.
- The opening between the right atrium and the right ventricle is guarded by a valve formed of three muscular flaps or cusps, the tricuspid valve, whereas a bicuspid or mitral valve guards the opening between the left atrium and the left ventricle.
- The flaps of both Bicuspid and Tricuspid valve are attached to Papillary muscles through Chordae Tendinae. These prevent reverting of the valves during contraction of ventricles.
- Bicuspid is the only valve in mammalian heart which always remains in contact with the pure (oxygenated) blood. All other type of valves come in contact with deoxygenated blood.
- The wall of the left ventricle, which supplies oxygenated blood to all body organs, is thickest of all chambers.
- Eustachian valve is present at the opening of the post caval and prevents the back flow of the blood. The major portion of this valve is vestigial.
- Thebasian valve is present at the opening of coronary sinus which receives deoxygenated blood from cardiac muscles.
- Semilunar valves (3 cusps) are present at the base of each aorta (systemic and pulmonary) with which prevents back flow of blood to the ventricles.
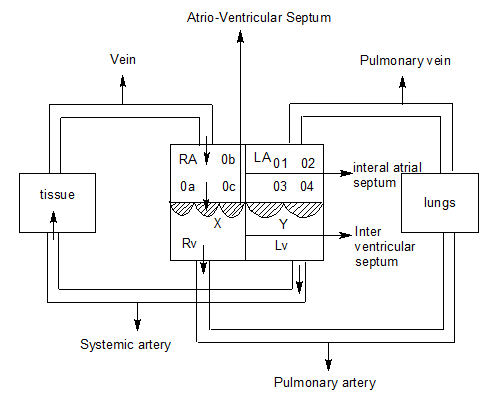
Heart Openings
- a, b, c Represents the opening of vena cava
- a. Opening of inferior vena cava (guarded with Eustachian valve)
- b. Opening of superior vena cava (without valve)
- c. Opening of coronary sinus (guarded with Thebasian valve)
- 1, 2, 3, 4 Opening of pulmonary vein in left Atrium (without valve)
- X. Tricuspid valve
- Y. Bicuspid (Mitral valve)
Arteries, Veins and Capillaries
Each artery has three coats, viz (i) Tunica externa (adventitia), (ii) Tunica media and (iii) Tunica interna (intima).
- Tunica externa mainly consists of white fibrous connective tissue (collagen fibres).
- Tunica media contains elastic fibres and smooth muscles.
- Tunica interna has endothelial layer (simple squamous epithelium) or intima layer with elastic fibres.
| Arteries | Veins |
| More elastic | Less elastic |
| Tunica media very thick | Tunica media thin |
| Lumen narrow | Lumen broader |
| Valves absent | Valves (semilunar) present in (longer) veins |
| Lie deeper in the body | Generally superficial |
| All, except pulmonary artery, carry oxygenated blood | All, except pulmonary vein, carry deoxygenated blood |
| Blood flow is jerky or discontinuous | Blood flow is continuous |
| These vessels carry blood away from the heart | These carry blood towards heart |
| They contain ~ 13% of the blood at a time | They contain ~ 65% of the blood at a time |
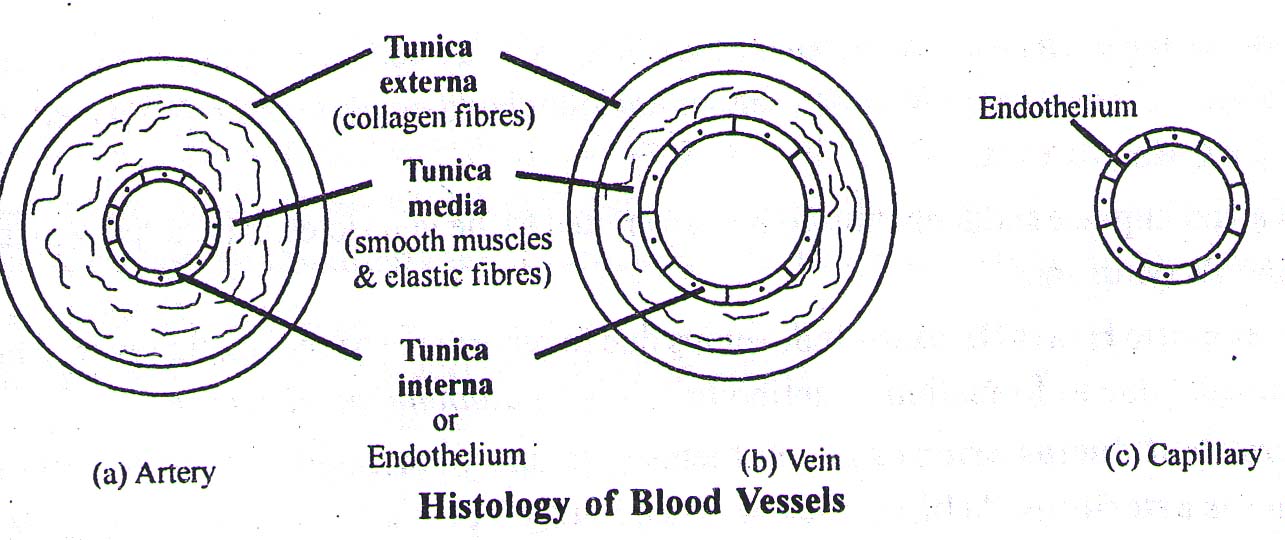
Capillaries
- Tunica externa and T. media are absent. There are no collagen fibres, no elastin fibres and no smooth muscles.
- Only endothelial lining with basement membrane is present.
- (The capillary network supplying outer layer of larger blood vessels is called vasavasorum)
Conduction System of Heart
Like all other vertebrates, in human also, the heart is Myogenic, i.e. the heart beat is generated by muscles and not nerves. Except molluscs, all invertebrates have neurogenic heart. The entire heart is made of cardiac muscles. A specialised cardiac musculature called the nodal tissue, is also distributed in the heart.
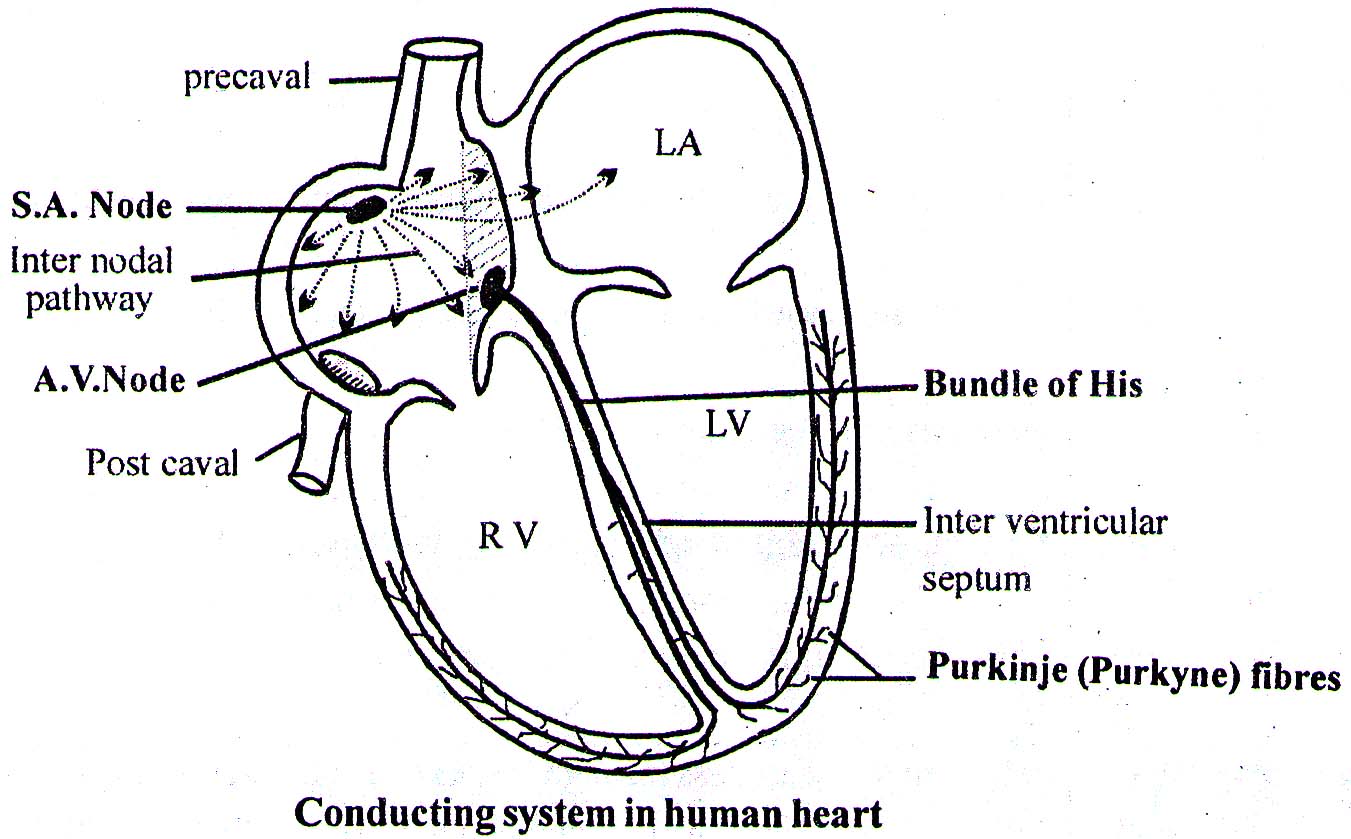
- In human, SA node is embedded in the right upper corner of Rt. atrium.
- The SAN can generate the maximum number of action potentials, i.e., 70-75 min⁻¹, and is responsible for initiating and maintaining the rhythmic contractile activity of the heart. Therefore, it is called the pacemaker.
- Atrio-ventricular node (AVN) is present in inter-atrial septum, close to Tricuspid valve.
- From AV node arises a bundle of specialized muscle fibres, called Atrio-ventricular bundle. This runs in the anterior part of inter-ventricular septum and then bifurcates into right and left bundle. The branches ramify in the walls of ventricles as Purkinje fibres. These fibres along with right and left bundles are known as bundle of HIS. Purkinje fibres are present in Endocardium of the heart wall. Action potential travels fastest in Purkinje fibres (4ms⁻¹).
Heart Beat
The rate of heart beat in a adult human is 70-75 times in a minute (average 72 times min⁻¹).
Cardiac Cycle
The single heart beat and its related activities of the heart are called One Cardiac cycle. It takes 0.8 sec (60 sec./72 beats) to complete one cardiac cycle. Each Cardiac cycle consists of 3-parts:
- Atrial systole (0.1 sec.): The SAN now generates an action potential which stimulates both the atria to undergo a simultaneous contraction – the atrial systole. This increases the flow of blood into the ventricles by about 30 per cent (active ventricular filling).
- Ventricular systole (0.3 sec.): Ventricular systole, increases the ventricular pressure causing the closure of tricuspid and bicuspid valves to produce first heart sound 'lubb', to prevent backflow of blood into the atria. As the ventricular pressure increases further, the semilunar valves are forced open, allowing the blood in the ventricles to flow through these vessels into the circulatory pathways.
- Joint Diastole (0.4 sec.): Atria and ventricles relax together, resulting in 70% passive filling of ventricle. The ventricles now relax (ventricular diastole) and the ventricular pressure falls causing the closure of semilunar valves which prevents the backflow of blood into the ventricles. It produces second Heart sound called 'Dup'.
- Joint diastole is followed by Atrial systole of next cardiac cycle.
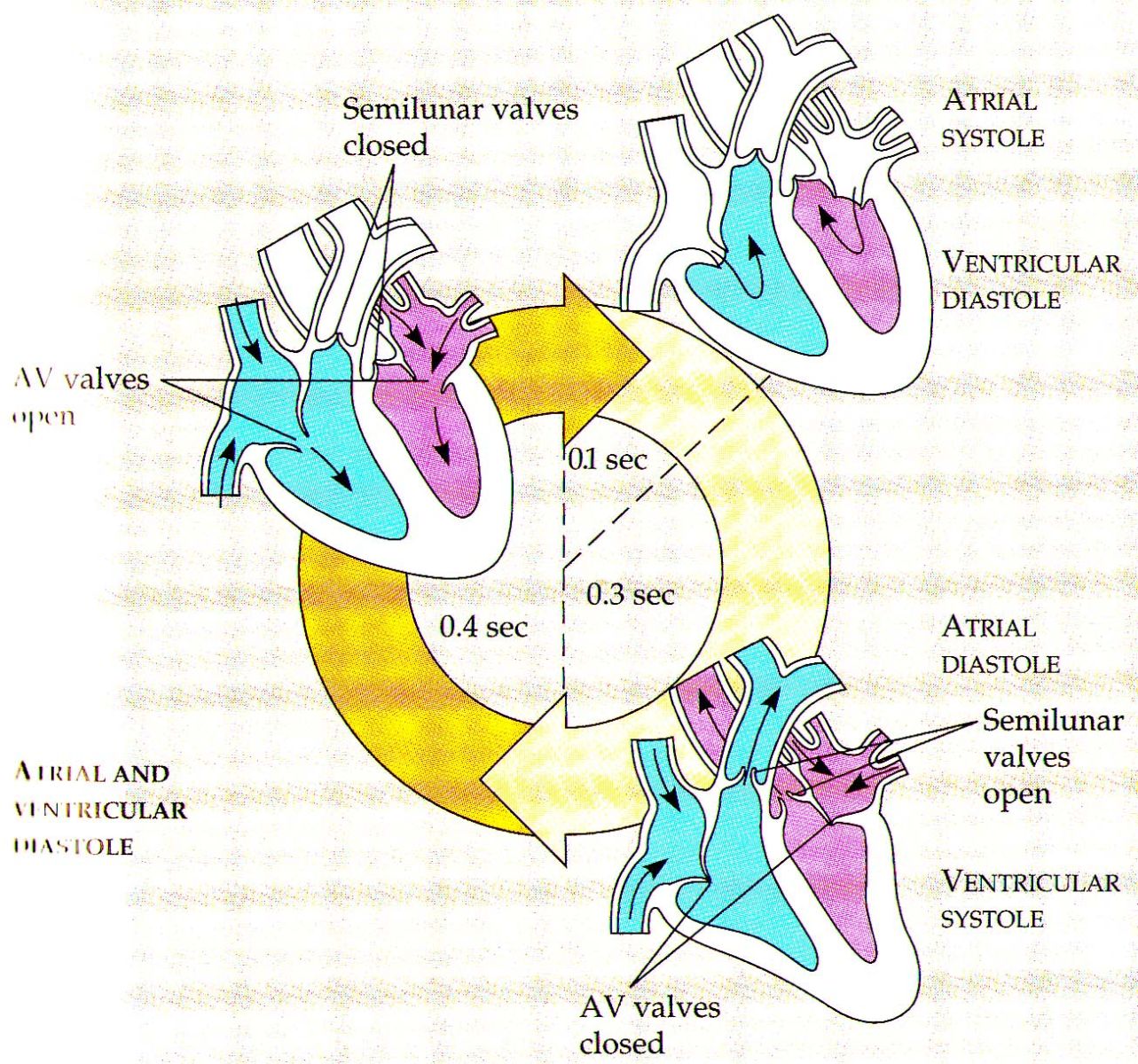
| Chamber | Systole | Diastole |
| Atrium | 0.1 sec. | 0.7 sec. |
| Ventricle | 0.3 sec. | 0.5 sec. |
Cardiac Output
- Stroke volume ~ 70 ml: It is the amount of blood pumped out from each ventricle per beat.
- Cardiac output ~ 5 LITRE: It is the output of the heart per unit time (70 ml × 72 beats per min.)
- The body has the ability to alter the stroke volume as well as the heart rate and thereby the cardiac output. For example, the cardiac output of an athlete will be much higher than that of an ordinary man.
- CO ∝ venous return (starling law)
- CO ∝ strength of ventricular contraction
Factors Affecting Heart Beat
- Heart beat increases during excitement, eating, exercise, fever and pregnancy.
- Heart beat decreases during sleep and shock.
- Heart beat is more in females than in males
- Heart beat increases with the increase of altitude (Heart beat ∝ altitude)
- The heart beat increases with the decrease of animal size (Heart beat ∝ 1/size). If elephant, human and mouse are compared, the heart beat will be highest in mouse and lowest in elephant.
- Heart beat ∝ 1/BP (except in exercises, in which both blood pressure (BP) and the rate of heart beat, increase)
Control of Heart Beat
a) Chemical Control
- Adrenaline: This hormone stimulates heart beat either directly or through sympathetic nervous system.
- Thyroxine: This increases metabolic rate and hence heart beat.
b) Nervous Control (Autonomic control)
- Accelerator centre: It functions through sympathetic nervous system (SNS) and increases heart beat by the secretion of epinephrine or adrenaline.
- Depressor centre: It functions through parasympathetic nervous system (PSNS) by the secretion of acetylcholine. It decreases heart beat.
E.C.G. (E.K.G.)
The instrument which records electrical activity of the heart muscles is called Electrocardiograph. The sketch obtained on the graph paper is called electrocardiogram (or electrocardiogram).
- Each peak in the ECG is identified with a letter from P to T that corresponds to a specific electrical activity of the heart.
- The P-wave represents the electrical excitation (or depolarisation) of the atria, which leads to the contraction of both the atria.
- The QRS complex represents the depolarisation of the ventricles, which initiates the ventricular contraction. The contraction starts shortly after Q and marks the beginning of the systole by counting the number of QRS complexes that occur in a given time period, one can determine the heart beat rate of an individual.
- The T-wave represents the return of the ventricles from excited to normal state (repolarisation). The end of the T-wave marks the end of ventricular systole.
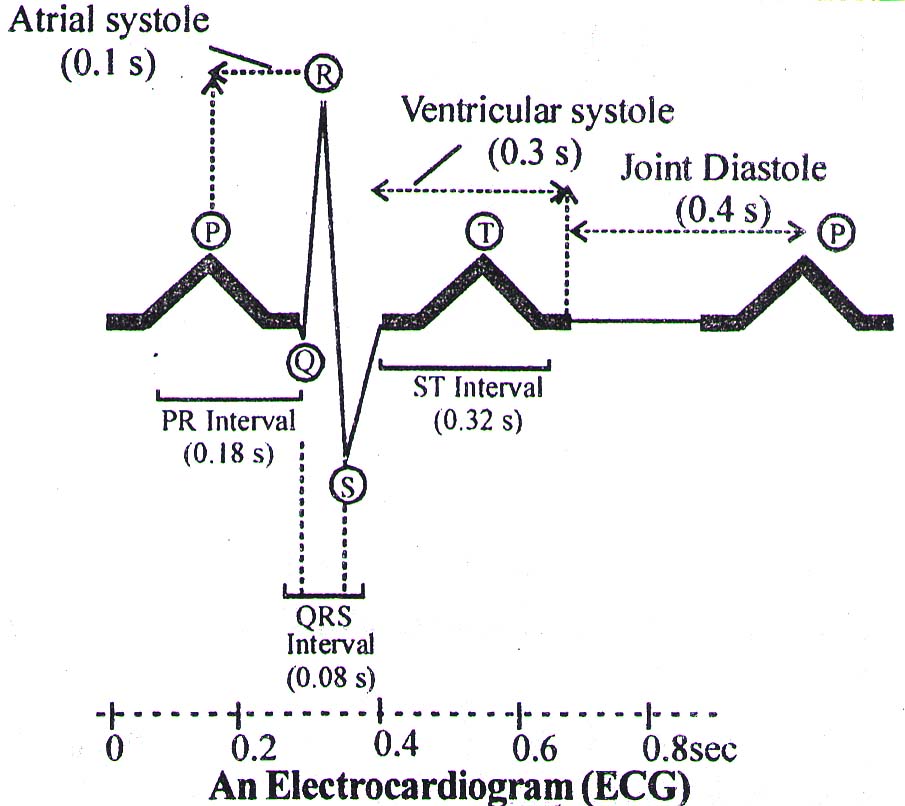
Intervals in Normal ECG
| Interval | Average Duration | Event |
| PR (or PQ) | 0.18 sec. (180 mili sec.) | Atrial depolarization and conduction through AV node |
| QRS | 0.08 sec (80 ms) | Ventricular depolarization and atrial repolarisation |
| ST | 0.32 sec (320 ms) | Ventricular repolarisation |
Blood Pressure
The pressure exerted by the blood on the walls of blood vessels is called blood pressure (BP). The blood pressure in all the arteries is relatively very high, but drops with distance away from the heart. BP is measured by Sphygmomanometer on Brachial artery of upper arm (generally of left side).
- BP decreases from arteries to veins (arteries > capillaries > veins)
| SP (mmHg) | DP (mmHg) | |
| Adult | 120 | 80 |
| Children | 90 | 55 |
| Old | 150 | 90 |
SP → Systolic Pressure DP → Diastolic pressure
- Pressure of 140/90 or more than this show Hypertension or High blood pressure. High blood pressure leads to heart diseases and also affects vital organs like brain and kidney.
- CO ∝ BP
- CO ∝ Resistance of blood vessel
- Increases in BP, decreases the rate of heart beat (Marey's law)
- BP ∝ 1/velocity of blood flow
- Increases in diameter of blood vessel two times, velocity increases 16 times
Pulse
Pulse is a wave of distension, i.e., a rhythmic expansion and relaxation (not contraction) of arteries.
- Pulse is felt at radial artery, of wrist.
- With the help of pulse the heart beat can be measured.
Pulse Pressure
- It is the difference between systolic and diastolic pressure.
- In normal adult the value of pulse pressure is 40 mm of Hg (120 mm – 80 mm)
Arterial System In Human
| Part of Aorta | Major Branch | General Regions or Organs Supplied |
| Ascending aorta | Right and left coronary arteries | Heart |
| Arch of aorta | Brachiocephalic artery | Right Upper limb, right sided of head |
| Left common carotid artery | Left side of head | |
| Left subclavian artery | Left upper limb | |
| Descending aorta (Thoracic aorta) | Bronchial artery | Bronchi |
| Pericardial artery | Pericardium | |
| Esophageal artery | Esophagus | |
| Mediastinal artery | Mediastinum | |
| Posterior intercostals artery | Thoracic wall | |
| Descending aorta (Abdominal aorta) | Celiac artery | Organs of upper digestive tract |
| Phrenic artery | Diaphragm | |
| Superior mesenteric artery | Portions of small and larger intestines | |
| Suprarenal artery | Adrenal gland | |
| Renal artery | Kidney | |
| Gonadal artery | Ovary or testis | |
| Inferior mesenteric artery | Lower portions of large intestine | |
| Lumbar artery | Posterior abdominal wall | |
| Middle sacral artery | Sacrum and coccyx | |
| Common iliac artery | Lower abdominal wall, pelvic organs and lower limb |
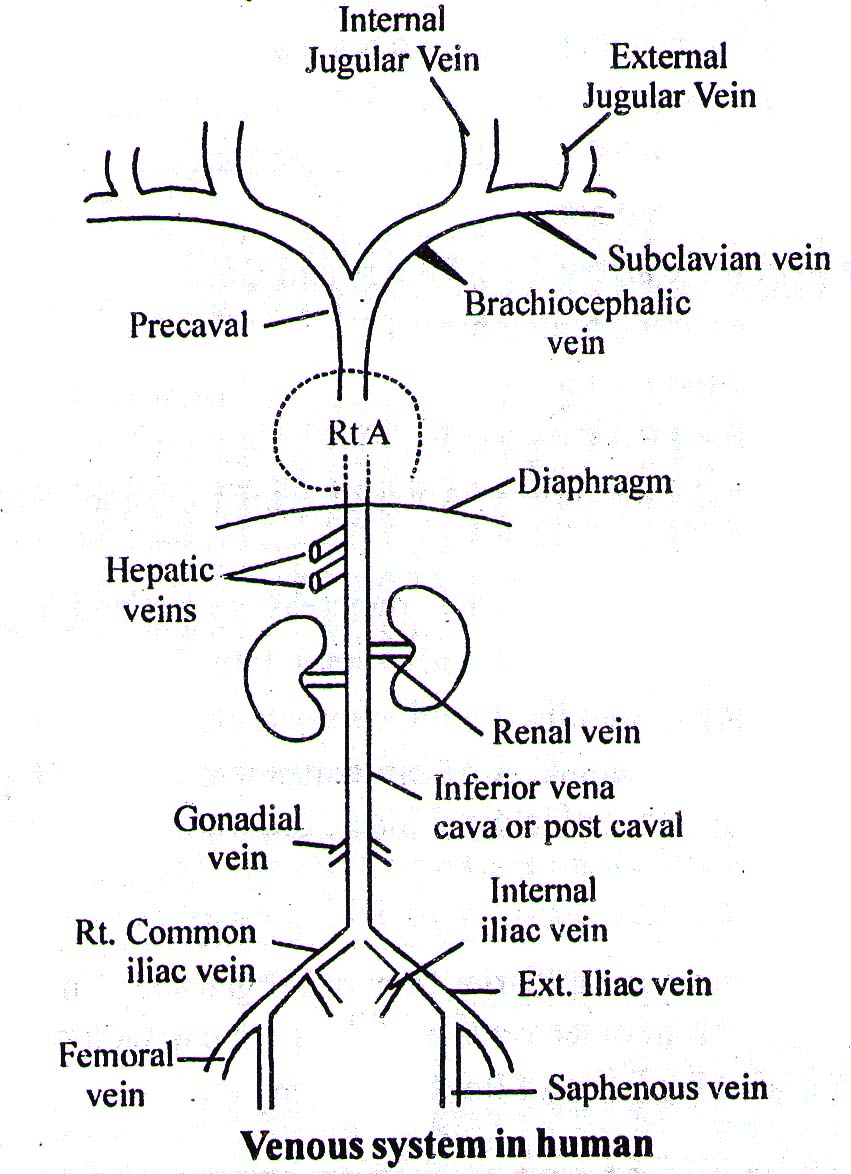
The Venous System
- Precaval or superior vanacava is formed by combination of 2-Brachiocephalic veins
- Brachiocephalic vein is formed by the union of internal jugular vein and subclavian vein. External jugular runs down to join subclavian vein.
- The venous blood from brain is collected by internal jugular vein.
- The subclavian vein (below clavicle bone) collects deoxygenated blood from arms.
- Postcaval or inferior venacava is formed by the joining of Rt. and Lt. common iliac vein.
- Hepatic vein, renal vein and gonadal veins join postcaval.
- From hind limbs the venous blood is collected through Femoral and Saphenous veins. The femoral vein ascends in to the abdominal region and become external iliac vein.
Portal System
Portal Vein
It is a vein that arises as capillaries from one organ and terminates as capillaries in the other organ. Portal vein is different from other veins as it does not carry blood directly to the heart. The system formed by portal veins is called Portal system.
Types of Portal System
Hypophyseal Portal System
- Such system is present between hypothalamus (the floor of diencephalons) and anterior pituitary.
- This portal system is meant for transferring the releasing factors (Hormones) from Hypothalamus to the Anterior pituitary.
Hepatic Portal System
- It is present in all vertebrates.
- It starts from alimentary canal and terminates into liver.
- It brings digestive end products to the liver before releasing them (in modified form) into the blood.
- Renal portal system is absent in human beings.
Diseases of Heart
- Angina pectoris: Pain in heart muscles, appearing as chest pain. It occurs due to conditions that affect the blood flow.
- Tachycardia: Increased rate of heart beat.
- Bradycardia: Decreased rate of heart beat.
- Heart attack: When symptoms such as breathlessness, palpitations, pain in the chest, unconsciousness appear suddenly.
- Heart Block: When heart beat is not passed to the ventricles properly. This is the defect of conducting system of the heart.
- Heart arrest: Sudden stoppage of impulse formation from the major nodal tissue, and hence heart stops beating.
- Heart failure: Heart failure means the state of heart when it is not pumping blood effectively enough to meet the needs of the body. It is sometimes called congestive heart failure because congestion of the lungs is one of the main symptoms of this disease.
- Arrythmia: It is irregular heart beat.
- Coronary thrombosis: It is due to formation of clot in coronary artery.
- Atherosclerosis (Coronary artery disease): Thickening of walls of blood vessels due to deposition of fat including cholesterol. Frequently causes Myocardial Ischaemia (inadequate flow of blood to a part of heart) leading to myocardial infarction (death or tissue due to lack of blood).
- Myocardial infarction: It is the death of a part of heart muscle following cessation of blood supply to it. It is acute heart attack.
- Arteriosclerosis: Hardening or loss of elasticity of arteries.