Respiration is a physiochemical process involving exchange of gases and oxidation of food material to release energy. It is a catabolic process that includes two parts:
- External Respiration: It includes intake of oxygen and removal of carbon-di-oxide from the body. It is also known as ventilation or breathing.
- Internal Respiration: It includes gaseous exchange between the cells and extracellular fluid, which results in utilization of oxygen and production of carbon-di-oxide, by the cells.
Respiratory structures in different animal groups
| Phylum/Group | Respiratory Structure |
| Protozoans, Poriferans, Coelenterates and Helminthes | Through body surface |
| Earthworm (Annelids) | Moist cuticle (cutaneous respiration) |
| Insect (Arthropods) | Tracheal system |
| Aquatic arthropods, Molluscs | Gills |
| Pisces, Cyclostomes | Gills |
| Amphibians | Moist skin, gills, lungs |
| Reptiles, Aves, Mammals | Lungs (pulmonary respiration) |
Respiratory System in Humans
The respiratory system consists of following important structures.
A pair of external nostrils
Nasal passage
- It contains hair for filtering out dust particles.
- Bowman’s glands (secrete mucus).
- Turbinals (bones) warm up the air.
- The sensory lining of nasal passage is called Schneiderian membrane.
A pair of internal nostrils
Pharynx
- It is a common passage for gut and respiratory tract.
- The opening between pharynx and larynx is called Glottis. It is closed by epiglottis during swallowing of food. However, the opening between Pharynx and Gut (Oesophagus) is different, and is called Gullet.
- The lateral sides of Nasopharynx contain openings of Eustachian tubes.
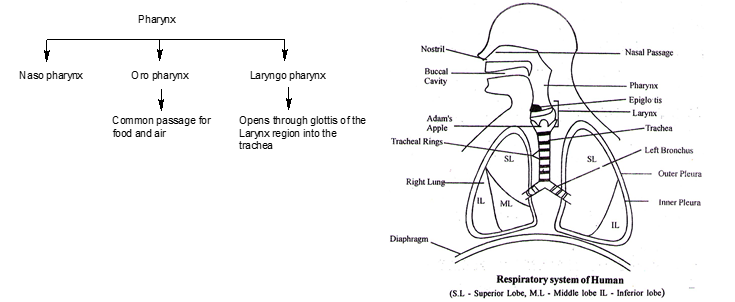
Larynx
- It is commonly called voice box or sound box.
- In humans it contains 9 cartilages – three paired and three unpaired. The unpaired cartilages include Thyroid, Cricoid and Epiglottis, while paired cartilages are Arytenoid, Corniculate and Cuneiform.
- Thyroid cartilage is collar shaped in males it forms Adam’s apple.
- During swallowing glottis is covered by a thin elastic cartilaginous flap called epiglottis, to prevent the entry of food into larynx.
Trachea
- It is a straight tube (length 12 cm) extending upto the mid thoracic cavity. It is located anterior to the oesophagous and extend from the larynx to the level of 5th thoracic vertebra.
- Tracheal lining is of pseudo-stratified epithelium
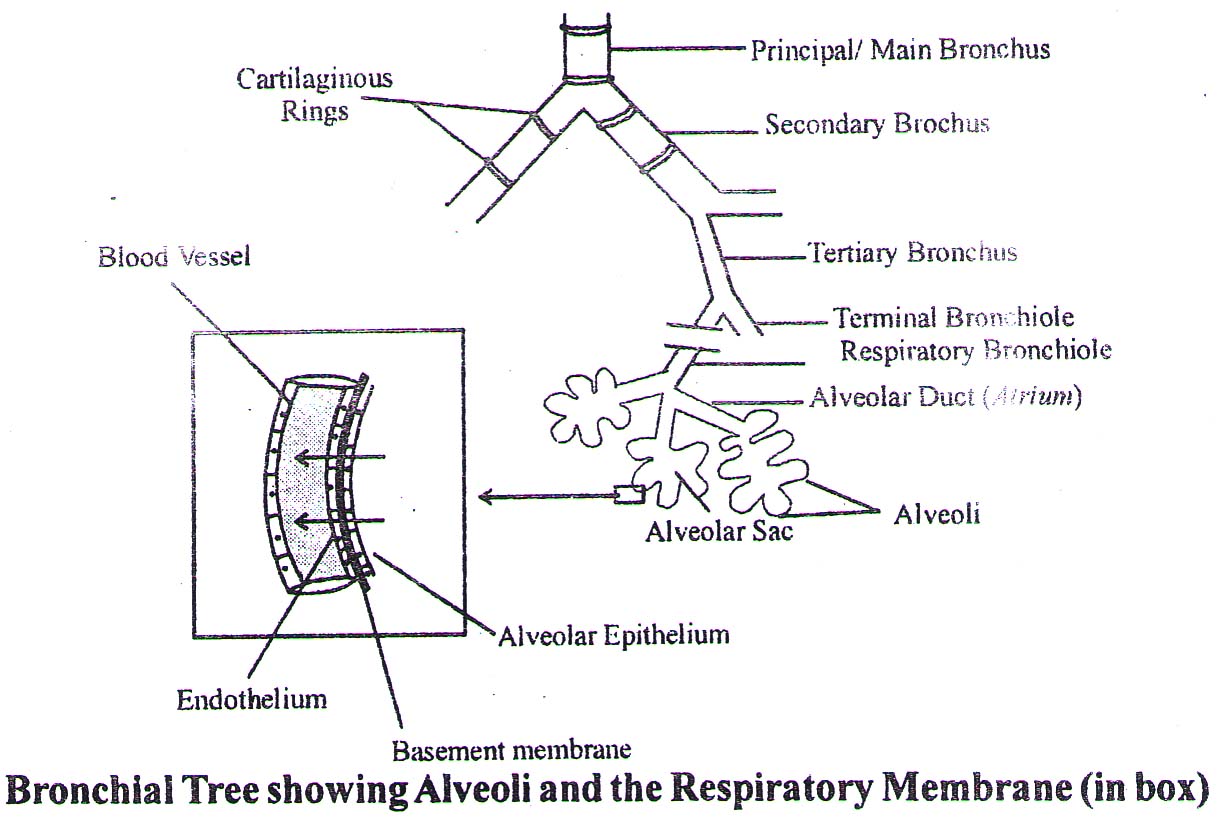
Bronchi, Bronchioles and Alveoli
- Trachea divides at the level of 5th thoracic vertebra into right and left primary bronchi. These further divide into secondary bronchi and tertiary bronchi.
- Bronchi divide into terminal bronchioles which in turn divide into respiratory bronchioles.
- Respiratory bronchioles branches into alveolar ducts forming alveolar sacs. Each alveolar sac is surrounded by Alveoli. The number of Alveoli in both the lungs is 300 to 350 million. Total surface area of alveoli is 70 – 100 m2. Inner lining of the alveoli is made up of simple squamous epithelium. Alveolar epithelium consist of type I alveolar cells, type II alveolar cells and dust cells (macrophages).
- Type II cells of aveoli and clara cells of respiratory bronchioles secrete surfactant (lecithin), which helps to keep the alveoli expanded.
- Epithelial wall of alveoli is richly supplied by blood capillaries.
- The exchange of gases occurs mainly through alveoli.
- The trachea, primary, secondary and tertiary bronchi, and initial bronchioles are supported by incomplete cartilaginous rings, made up of hyaline cartilage which prevents its collapsing. These cartilaginous rings are dorsally incomplete.
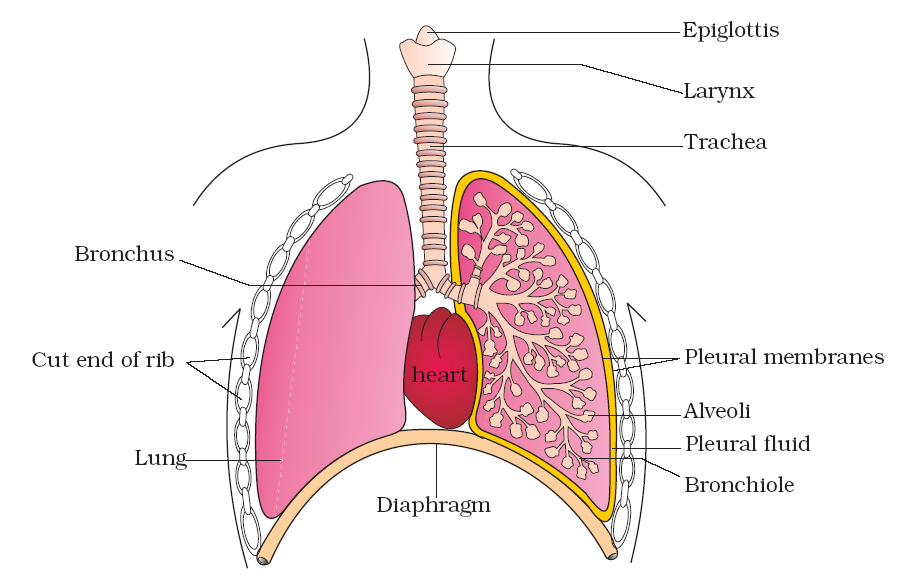
Lungs
- Lungs in human are solid and spongy and are located in the thoracic cavity – which is anatomically an air tight chamber. The thoracic chamber is formed dorsally by the vertebral column, ventrally by the sternum, laterally by the ribs and on the lower side by the dome-shaped diaphragm.
- Each lung is surrounded by two membranes called pleura. The outer pleural membrane is in close contact with the thoracic lining whereas the inner pleural membrane is in contact with the lung surface. Right and left lung consists of three and two lobes, respectively.
The cavity between two pleura (pleural cavity) is filled with a fluid (pleural fluid) which reduces friction during breathing.
Diagrammatic view of human respiratory system (Sectional view of the left lung is also shown) Diaphragm
- It is a muscular partition between thorax and abdomen of all mammals.
- It is dome shaped at rest.
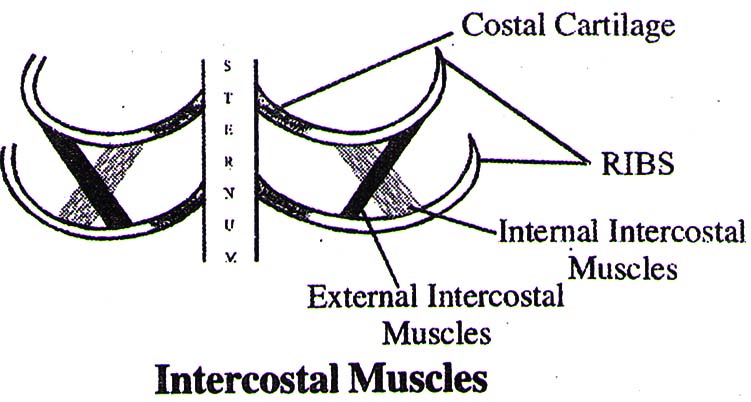
Ribs
- Number of ribs in human is 12 pairs.
- In between ribs two sets of inter-costal muscles are present. i.e., External intercostal muscles and Internal inter-costal muscles. These muscles help in the movement of ribs during breathing.
Mechanism of breathing
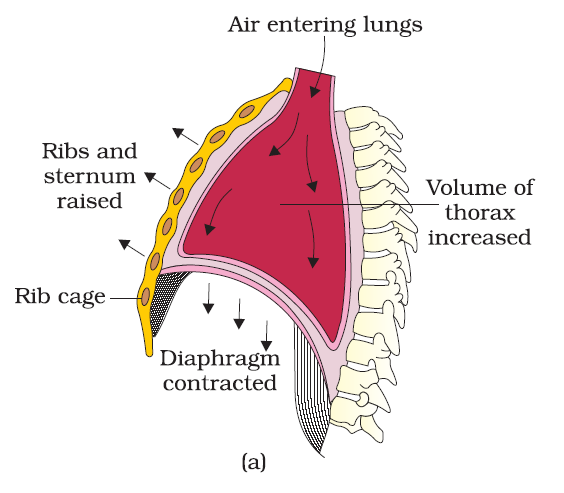
(a) Inspiration
- It is an active process which involves contraction of diaphragm (Phrenic muscle) and External Inter Costal Muscles (EICM).
- Diaphragm is responsible for 80% of breathing volume during quiet normal breathing and EICM are responsible for (20-25%).
- The diaphragm-muscles contract and the dome shape of diaphragm changes to flat. With the contraction, the lower surface of the lungs is also pulled downward.
- The external inter-costal muscles contract and the ribs move outward upward and formation to increase the volume of thoracic cavity.
- Lungs expand and air is drawn into the lungs. The lungs in human, like other mammals, are negative (-ve) pressure type. Inspiration can occur if the pressure within the lungs (intra-pulmonary pressure) is less than the atmospheric pressure
(b) Expiration
- Quiet expiration is a passive process or elastic recoil process, which occurs due to relaxation of diaphragm and EICM.
- The diaphragm becomes dome shaped again.
- In forced expiration, the internal inter-costal muscles and abdominal muscles contract. This is an active process.
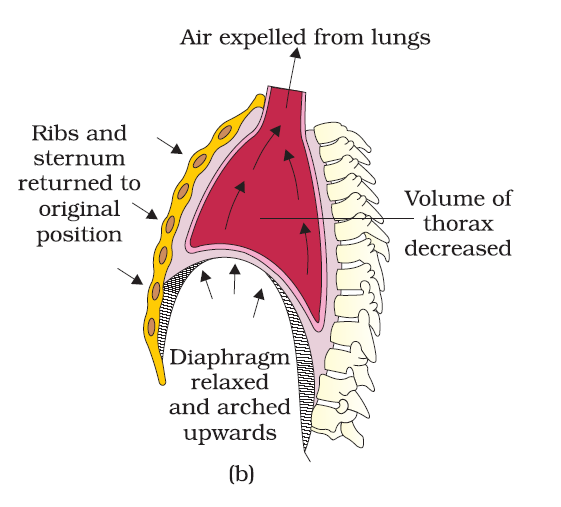
Mechanism of breathing showing : (a) inspiration (b) expiration Breathing rate
- 12–16 / min.
- In newly born child the breathing rate is ~ 40/min.
Respiratory volumes and capacities
The volume of air involved in breathing movements can be estimated by using a spirometer which helps in clinical assessment of pulmonary functions
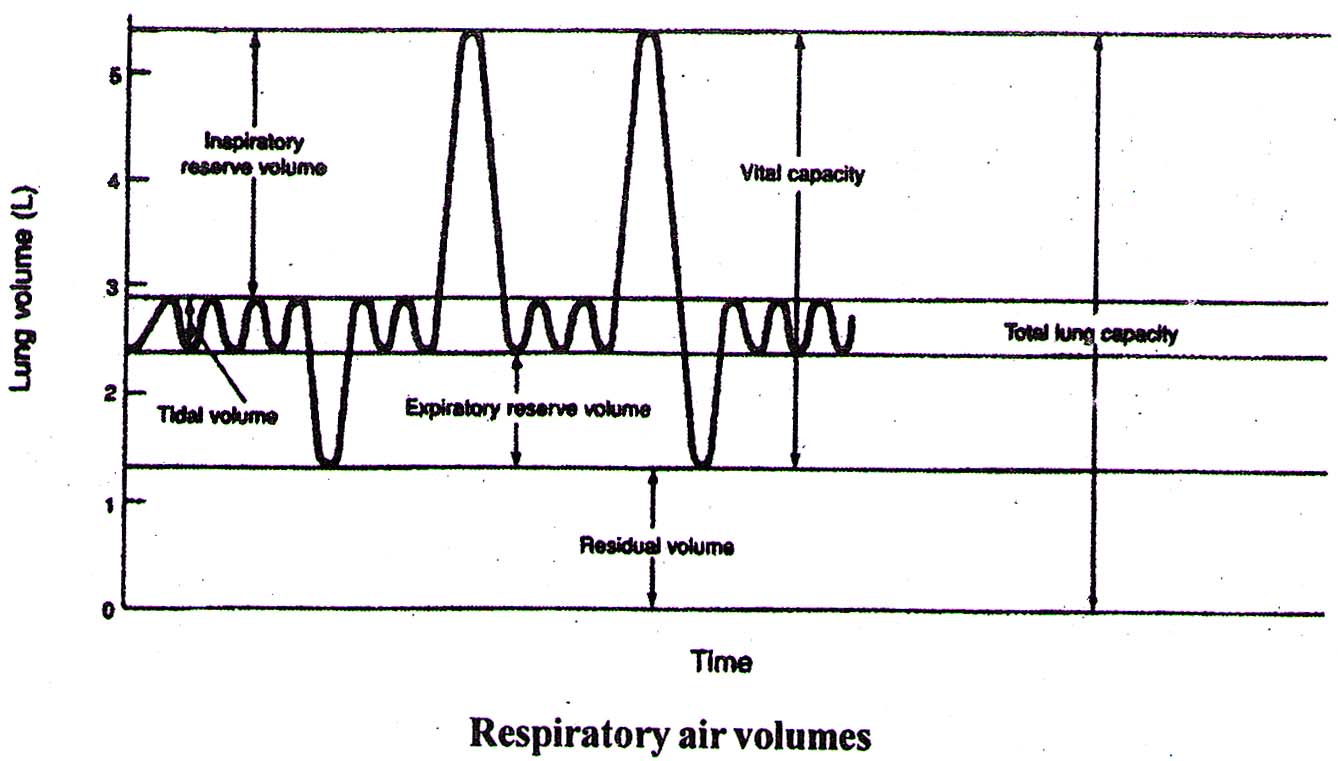
| Lung | ||||||
| Volume | Capacities | |||||
| Tidal volume (T.V) | 500 ml | Is the air that moves into the lung with each normal inspiration or the volume of air that moves out of lung with each expiration | Inspiratory capacity I C = TV + IRV | 3 – 3.5 L | Total amount of air that can be breathed in with maximum inspiratory effort | |
| Inspiratory reserve volume (IRV) | 2.5 – 3 L | The air inspired with a maximal inspiratory effort in excess of tidal volume | Vital capacity VC = TV + IRV + ERV | 3.5 – 5 L | Maximal amount of air that can be expelled out force fully after a maximal (deep) inspiration | |
| Expiratory reserve volume (ERV) | 1 – 1.1L | The air expelled with a maximal expiratory effort in excess of tidal volume | Functional residual capacity FRC = ERV + RV | 2.5 L | It is the volume of air remaining in the lungs after normal expiration (after normal tidal expiration) | |
| Residual Volume (RV) | 1.5 L | The amount of air remaining in the lungs even after forced expiration | Total lung capacity TLC = TV + IRV + ER V + RV | 5 – 6 L | The amount of air present in the lungs after a maximal inspiration. This is the maximum volume to which the lungs can be expanded. | |
Dead air space (anatomical dead space) = 150 ml The amount of air present in trachea, bronchi and bronchioles, which is not used in exchange of gases.
Mechanism of Respiration
Respiration involves the following steps:
- Breathing or pulmonary ventilation by which atmospheric air is drawn in and CO2 rich alveolar air is released out.
- Diffusion of gases (O2 and CO2) across alveolar membrane.
- Transport of gases by the blood.
- Diffusion of O2 and CO2 between blood and tissue fluid.
- Utilisation of O2 by the cells for catabolic reactions and resultant release of CO2
Exchange of gases
Diffusion capacity is the volume of gas which diffuses through the respiratory membrane per minute for a pressure difference of 1 mm of Hg. It is dependent on partial pressure and solubility of gases.
CO2 > O2 > N2 (The diffusing capacity of CO2 is 20 times greater to that of O2 and that of O2 is 2 times more than N2). Solubility of gases as well as the thickness of the respiratory membrane involved in diffusion are also some important factors that can affect the rate of diffusion.
The diffusion membrane is made up of three major layers namely, the thin squamous epithelium of alveoli, the endothelium of alveolar capillaries and the basement membrane in between them. However, its total thickness is much less than a millimetre.
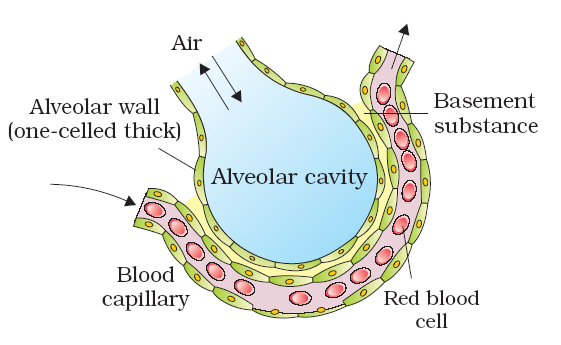
A diagram of a section of an alveolus with a pulmonary capillary
Pressure contributed by an individual gas in a mixture of gases is called partial pressure. It is represented as pO2 for oxygen and pCO2 for carbon dioxide.
Partial Pressures (in mm Hg) of Oxygen and Carbon dioxide at Different Parts Involved in Diffusion in Comparison to those in Atmosphere
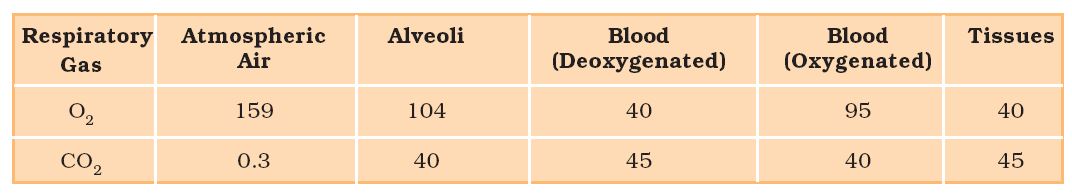
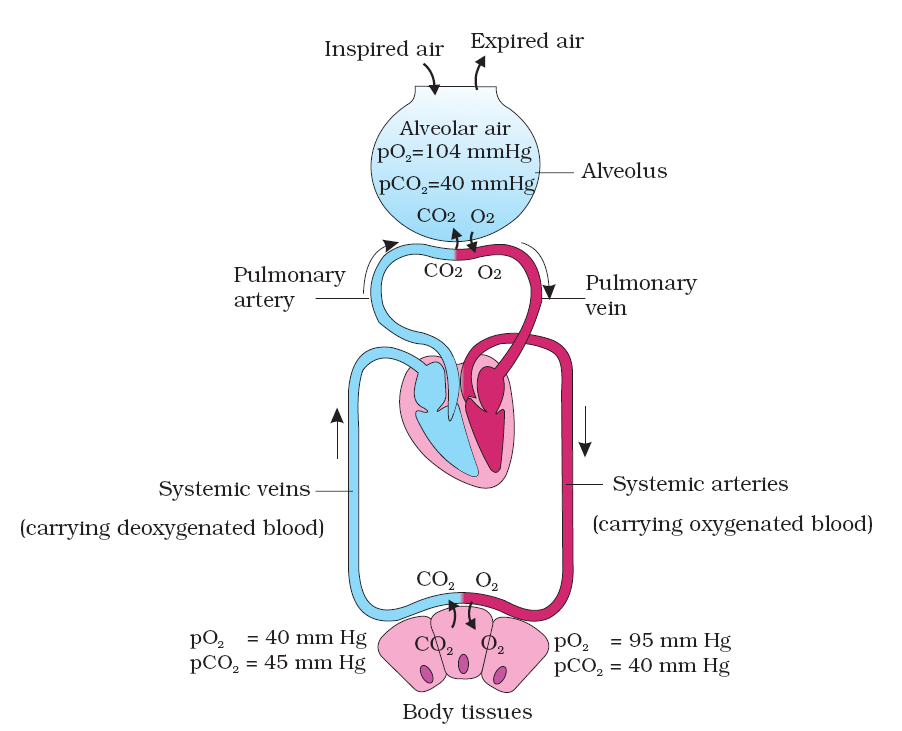
Diagrammatic representation of exchange of gases at the alveolus and the body tissues with blood and transport of oxygen and carbon dioxide
Transportation of Gases
Combination of Oxygen & CO2 with Hb Oxygen does not combine with two positive bonds of iron in the Hb molecule but it binds loosely with one of the so called co-ordination bonds of iron atom which is extremely loose & so the combination is easily reversible. CO2 combine with amino group of the Hb molecule. Each HB molecule has = 4 Polypeptide chains (a2, b2) = 4 Iron atoms = 4 molecules of O2 or 8 atoms of O2
Transportation of Oxygen
- Through RBCs (in combination with haemoglobin as oxyhaemoglobin) = 97 – 98%
- Through blood plasma (in dissolved form) =2 – 3%
- 1 gm of haemoglobin combines with 1.34 ml of oxygen
- 100 ml of blood (having ~ 15 g of hemoglobin) carries 19.4 ml of oxygen.
- Haemoglobin combines with oxygen to form oxyhaemoglobin. This process is called oxygenation and not oxidation as ferrous form of heam remains as ferrous.
- Oxygen carrying capacity of blood is – 20 ml/100 ml
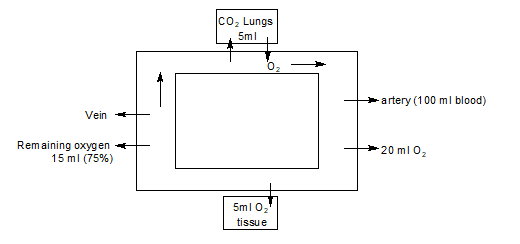
- 100 ml of oxygenated blood can deliver around 5 ml of O2 to the tissues under normal physiological condition.
- During one round through the body about 25% of oxygen is dissociated from oxyhaemoglobin and about 75% of oxygen is still associated with hemoglobin in venous blood.
Oxyhaemoglobin dissociation curve
- Saturation of haemoglobin plotted against the partial pressure of oxygen gives a Sigmoid (S-shaped) curve. This curve is called the Oxygen dissociation curve. Figure given here is highly useful in studying the effect of factors like pCO2, H+ concentration, etc., on binding of O2 with haemoglobin.
- Increase in 2, 3 DPG lower O2 affinity of Hb. 2, 3 DPG is most abundant organic phosphate in RBC’s & is synthesized from glycolytic intermediates.
Shifting of oxyhaemoglobin dissociation curve
- Factors increasing 2, 3 DPG Levels (right shift)
- Hypoxia (High altitude)
- High temperature
- High H+ (Bohr’s Theory – A rise in pCO2 or falls in pH decreases oxygen affinity of haemoglobin which shifts the curve to right.)
- Pregnancy · Exercise · Anemia
- Factors decreasing 2, 3 DPG Levels (Left shift)
- Stored blood
- Fetal hemoglobin
- Hyper ventilation
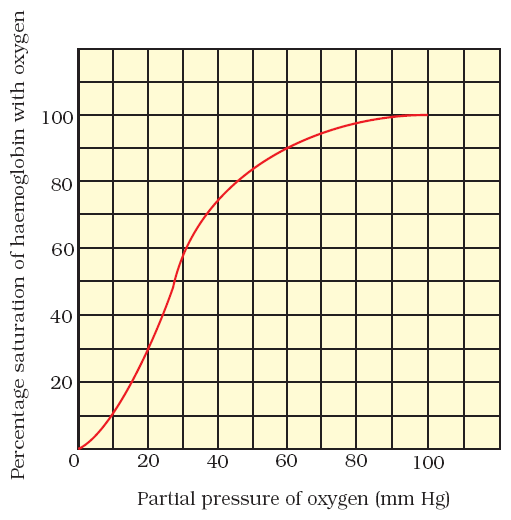
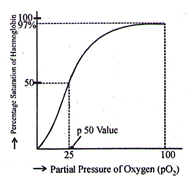
Oxygen Dissociation Curve
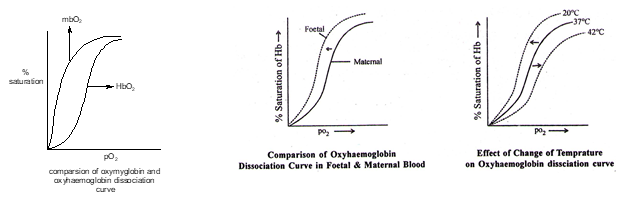
p50 Value
- The partial pressure of oxygen at which 50% of haemoglobin gets saturated is called p50 value.
- In normal adults, the p50 value is ~ 25 mm of Hg. In foetus since the affinity of haemoglobin is higher than that of adult the p50 value is lower and curve is on left hand side
Oxyhaemoglobin Dissociation Curve
Carbon Dioxide Transport There are 3 ways in which carbon dioxide is transported in the blood:
- Dissolved CO2
- Carbon dioxide is much more soluble in blood than oxygen.
- About 7 % of carbon dioxide is transported unchanged, simply get dissolved in the plasma
- Bound to Haemoglobin
- Carbon dioxide combines reversibly with haemoglobin to form carbaminohaemoglobin. Carbon dioxide does not bind to iron, as oxygen does, but to amino groups on the polypeptide chains of haemoglobin.
- Carbon dioxide also binds to amino groups on the polypeptide chains of plasma proteins
- About 20-25% of carbon dioxide is transported bound to haemoglobin.
- Bicarbonate Ions (HCO3- )
- In the form of Bicarbonates (through RBCs and Plasma) = 70% in the form of NaHCO3 in blood plasma.
- Carbon dioxide enters red blood cells in the tissue capillaries where it combines with water to form carbonic acid (H2CO3). This reaction is catalysed by the enzyme carbonic anhydrase, which is found in the red blood cells. Carbonic acid then dissociates to form bicarbonate ions (HCO3- ) and hydrogen ions (H+).
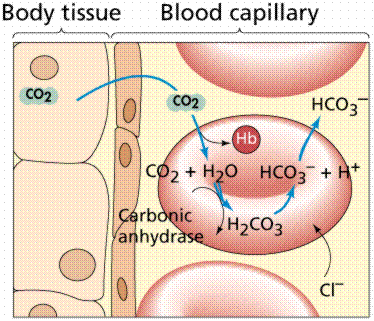
This diagram shows CO2 diffusion in the tissue fluid and blood
CO2 + H2O H2CO3 HCO3– + H+
- This reaction also occurs outside the red blood cells, in the plasma, but is much slower due to lack of carbonic anhydrase.
- The hydrogen ions, formed from the dissociated carbonic acid, combine with the haemoglobin in the red blood cell.
- Bicarbonate ions diffuse out of the red blood cells into the plasma while chloride ions (Cl-) diffuse in to take their place. This is known as the chloride shift or Hamburger’s Phenomenon
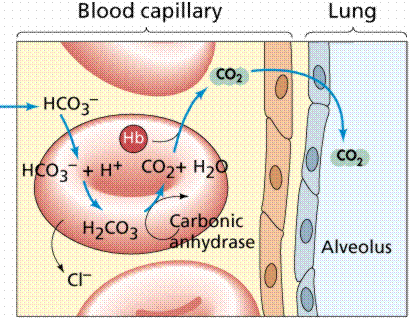
- The diagram above shows the reversal of the reactions which occur at the level of lungs. Bicarbonate ions enter the red blood cells and combine with hydrogen ions to form carbonic acid. This is broken down into carbon dioxide and water. Carbon dioxide diffuses out of the red blood cells and then into the alveoli.
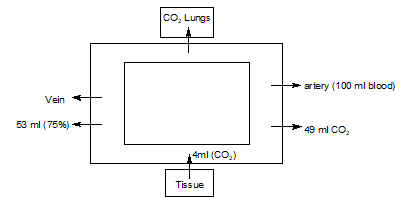
- Every 100 ml of deoxygenated blood delivers approximately 4 ml of CO2 to the alveoli.
Haldane’s Effect – Deoxyhaemoglobin (Hb) binds with more H+ than oxyhaemoglobin (HbO2) does. The deoxyhaemoglobin present in venous blood, thus, can carry more CO2 than oxyhaemoglobin. (The oxyhaemoglobin on the other hand is acidic and releases more H+)
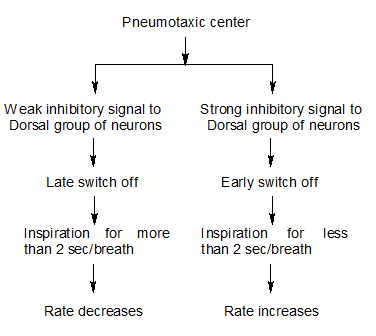
Regulation of Respiration
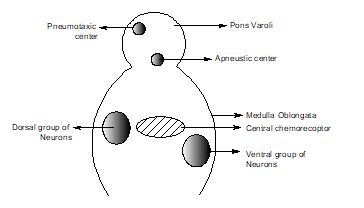
Respiratory Centers Regulating Breathing
- Voluntary Breathing or Conscious Breathing is controlled by Cerebral cortex via corticospinal tract.
- Involuntary Breathing centre is located in Medulla and Pons
| Neural Control of Breathing | ||
| Medullary System | Pontine and Vagal influences | |
|
|
|
| Chemical control on Respiratory Centre (Via) | ||
| Central chemoreceptors | Peripherial chemoreceptors | |
|
|
|
Important Terms and Disorders of Respiratory System
- Eupnea – It is normal breathing rate (12 ~ 15 per minute)
- Hypopnea – Decrease in breathing rate
- Hyperpnea – Increase in breathing rate
- Dyspnea – Distressed breathing or breathing with difficulty.
- Hypoxia – Lack of oxygen at tissue level. This term is preferred over Anoxia.
- Anoxia – No oxygen at tissue level.
- Asphyxia – Suffocation due to lack of oxygen and retention of CO2. It is produced by occlusion of the air way, acute hypercapnia and hypoxia developed together. (Asphyxia = Hypoxia + Hypercapnia)
- Cyanosis – Bluish or violet colouration of skin and the mucous membrane. This develops due to the presence of excessive amount of reduced haemoglobin or partially deoxygenated blood, or due to inadequate amount of oxygen in the blood. It develops at low temp. when carbonic anhydrase (enzyme) becomes inactive.
- Emphysema – Irreversible distension of the respiratory bronchioles, alveolar sacs and alveoli. The wall separating adjacent alveoli break down and air remains filled even after expiration. It develops mainly due to tobacco (cigarette) smoking.
- Asthma – It is in allergic disorder. The bronchioles constrict due to spasm of smooth muscles and expiration becomes difficult.
- Hay fever – It is an allergic disorder of nasal lining. It develops due to hypersensitivity of the lining to pollen grains or other foreign particles. There is an episode of sneezing that begins following allergy.
- Atelectasis – It is inability of lungs to expand at birth. This is mainly due to the deficiency of surfactant. In normal cases the surfactant (a phospholipid, lecithin) reduces tension at alveolar surface and the effort to expand the lungs at birth is reduced.
- Occupational lung diseases (Diseases of industrial workers) – Disease due to inhalation of organic and inorganic pollutants is called Pneumoconiosis. Long exposure can give rise to inflammation leading to fibrosis (proliferation of fibrous tissues) and thus causing serious lung damage. Workers in such industries should wear protective masks.
- Decompression Sickness (Bends diseases, Diver’s paralysis, caisson disease) When a diver gradually ascends from a dive, the nitrogen, dissolved at high pressure under water, diffuses from the tissues into the lungs and no harmful effects are noticed; but if the ascent is rapid then N2 escapes from the tissues and blood, in the form of bubbles, causing decompression sickness. These bubbles cause severe pain in joints. In the blood, the bubbles obstruct the arteries to the brain, spinal cord or other parts causing paralysis.
- CO-poisoning – Haemoglobin has much more, about 250 times more affinity for CO than for oxygen. In the presence of CO, it forms stable compound called carboxyhomoglobin and decreases oxygen availability for body tissues. It leads to asphyxiation and in extreme cause leads to death.