What is Gametogenesis?
Gametogenesis is the fundamental biological process responsible for the formation of male and female gametes (reproductive cells) from primitive germ cells. This essential reproductive mechanism includes two distinct processes: spermatogenesis (formation of male gametes) and oogenesis (formation of female gametes). Understanding gametogenesis is crucial for comprehending human reproduction and forms a vital component of CBSE Class 12 Biology curriculum.
Spermatogenesis: Formation of Male Gametes
Overview of Spermatogenesis
Spermatogenesis is the complex process of sperm cell development that begins at puberty and continues throughout adult life, gradually declining with age. This continuous process ensures the production of functional male gametes capable of fertilization.
The Four Phases of Spermatogenesis
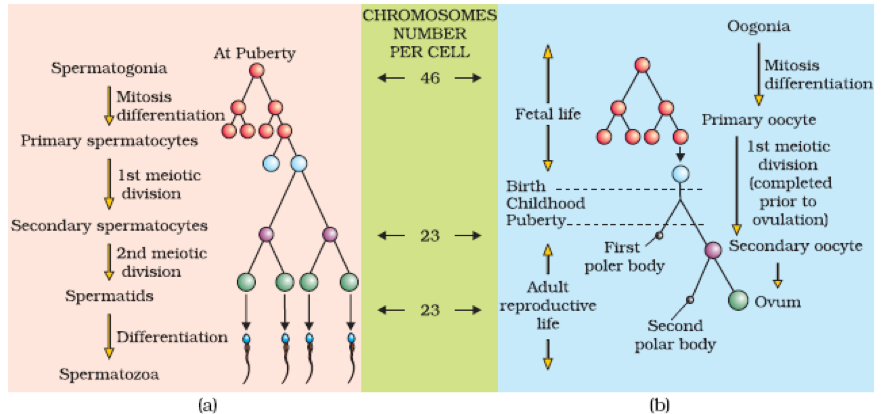
Phase 1: Mitotic Division of Spermatogonia
The process begins with spermatogonia, which are derived from primordial germ cells. These cells undergo continuous mitotic divisions to produce two distinct types:
- Spermatogonia A: Act as reserve stem cells, maintaining the pool of undifferentiated cells
- Spermatogonia B: Enter the growth phase and differentiate into primary spermatocytes
Phase 2: Formation of Secondary Spermatocytes
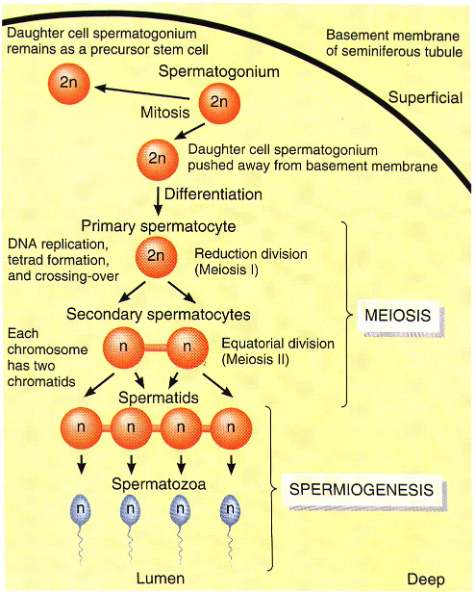
Primary spermatocytes undergo the first meiotic division (reductional division), resulting in:
- Chromosome reduction from diploid (44 + XY) to haploid (22 + X or 22 + Y)
- Formation of secondary spermatocytes
- Important: 50% of secondary spermatocytes carry X chromosome, while 50% carry Y chromosome
Phase 3: Formation of Spermatids
Each secondary spermatocyte undergoes the second meiotic division (equational division), producing:
- Two haploid spermatids from each secondary spermatocyte
- Four spermatids total from each original primary spermatocyte
Phase 4: Spermiogenesis (Formation of Spermatozoa)
Spermiogenesis is the transformation process where spermatids develop into mature spermatozoa through remarkable structural and physiological changes.
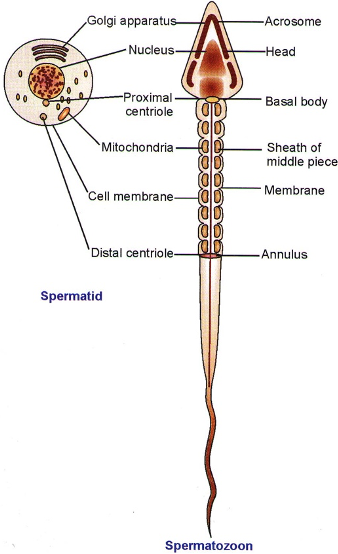
Structural Changes During Spermiogenesis
Nuclear Modifications
- Nucleus becomes compact through removal of nuclear sap and RNAs
- Transforms from spherical to anteriorly pointed structure
- Contains genetic material essential for fertilization
Golgi Body Reorganization
- Scattered Golgi bodies assemble at the anterior nucleus
- Secretory granules fuse to form the acrosome
- Acrosomal vesicle develops as a protective head cap
- Acrosome contains enzymes (hyaluronidase and proteinases) for egg penetration
Centrosome Development
- Both centrioles move to the posterior end of nucleus
- Form proximal and distal centrioles
- Distal centriole microtubules elongate to create axial filament
- Axial filament becomes part of middle piece and tail
Mitochondrial Organization
- All mitochondria fuse end-to-end forming mitochondrial sheath
- Arrange spirally around anterior axial filament
- Create the middle piece structure
- Spirally arranged mitochondria termed nebenkern
- Provide ATP for sperm locomotion
Mature Sperm Structure
A fully developed spermatozoon consists of three distinct regions:
1. Head
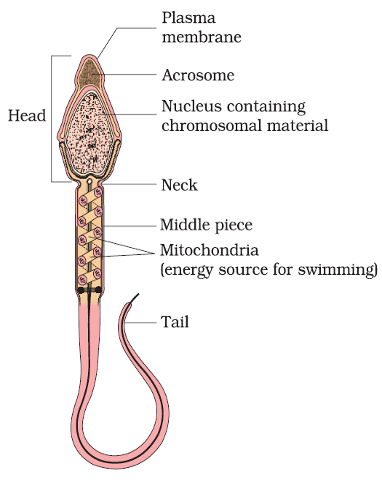
- Contains condensed nuclear material
- Houses the acrosome (specialized lysosome)
- Acrosome enzymes facilitate egg penetration
2. Middle Piece
- Packed with mitochondria arranged spirally
- Generates ATP for sperm motility
- Connects head to tail region
3. Tail
- Functions as a typical flagellum
- Propels sperm through female reproductive tract
- Essential for sperm mobility and fertilization
Spermiation Process
After spermiogenesis completion, sperm heads become embedded in Sertoli cells and are finally released from seminiferous tubules through spermiation. This process ensures proper sperm maturation and release.
Sperm Production Statistics
- Daily production: Approximately 120 million sperm cells
- Maturation time: Average of 74 days from germ cell to mature sperm
- Storage locations: Epididymis and ampulla of vas deferens
- Fertility duration: Maintained for approximately one month
- Capacitation: Final maturation occurs in female genital tract
Hormonal Control of Spermatogenesis
Hormonal Cascade
The hormonal regulation of spermatogenesis involves a sophisticated endocrine system:
Hypothalamic-Pituitary Axis
- GnRH (Gonadotropin Releasing Hormone): Released by hypothalamus at puberty
- Anterior Pituitary Response: Stimulated to secrete gonadotropins
- LH (Luteinizing Hormone): Acts on Leydig cells
- FSH (Follicle Stimulating Hormone): Acts on Sertoli cells
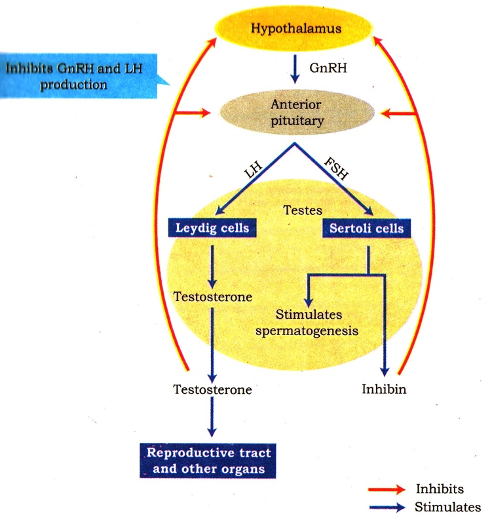
Target Cell Actions
- Leydig Cells: LH stimulates androgen synthesis and secretion
- Androgens: Stimulate spermatogenesis process
- Sertoli Cells: FSH stimulates factors supporting spermiogenesis
Feedback Mechanisms
The hormonal control operates through negative feedback loops ensuring optimal hormone levels for continuous sperm production.
Oogenesis: Formation of Female Gametes
Overview of Oogenesis
Oogenesis is the process of ovum (egg) formation from primitive germ cells in females. Unlike spermatogenesis, oogenesis involves prolonged developmental phases and cyclical ovulation.
Stages of Oogenesis
Fetal Oogenesis
- Begins by 10 weeks of gestation in fetal ovaries
- Oogonia proliferate through mitosis
- Transform into primary oocytes
- Primary oocytes enter prolonged meiotic arrest (diplotene stage)
- Remain arrested until ovulation at puberty
Primordial Follicle Formation
- Primary oocytes become surrounded by single layer of flat granulosa cells
- Form primordial follicles
- Granulosa cells derived from ovarian cortical cell proliferation
Primary Follicle Development
- Granulosa cells become cuboidal
- Primary oocyte enlarges significantly
- Many follicles degenerate from birth to puberty
- Only 60,000-80,000 primary follicles remain at puberty in each ovary
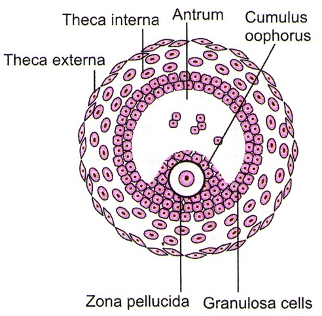
Secondary Follicle Formation
- Primary follicles acquire multiple granulosa cell layers
- Develop thecal layers
- Theca folliculi formed by ovarian cortex stromal cells
- Enhanced structural organization
Tertiary Follicle Development
- Multilayered granulosa cells secrete follicular fluid
- Antrum (cavity) forms in stratum granulosum
- Theca organizes into:
- Theca interna (inner layer)
- Theca externa (outer layer)
- Primary oocyte completes first meiotic division
- Unequal division produces:
- Large haploid secondary oocyte
- Small first polar body
- Secondary oocyte retains nutrient-rich cytoplasm
Graafian Follicle Maturation
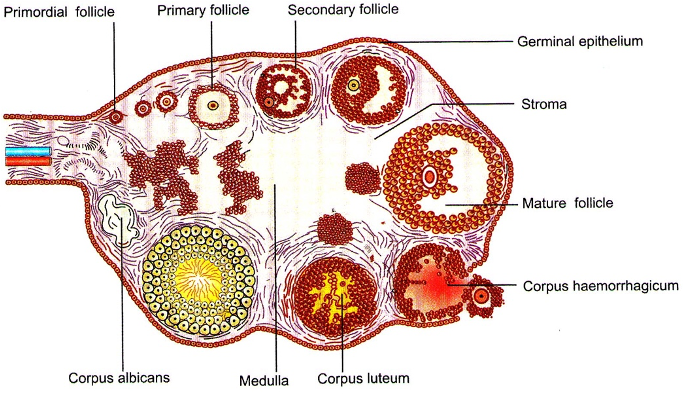
- Occurs around 7th day of sexual cycle
- One tertiary follicle enlarges in response to gonadotropins
- Forms mature Graafian (antral/vesicular) follicle
- Prepares for ovulation
Ovulation Process
Ovulation is the release of secondary oocyte from the ovary following Graafian follicle rupture into the peritoneal cavity. Typically occurs 14 days after menstruation onset in a normal 28-day cycle.
Key Differences: Spermatogenesis vs Oogenesis
| Aspect | Spermatogenesis | Oogenesis |
|---|---|---|
| Timing | Continuous from puberty | Cyclical from puberty |
| Location | Seminiferous tubules | Ovarian follicles |
| Gamete Production | ~120 million daily | One per cycle |
| Meiotic Completion | Both divisions complete | Second division after fertilization |
| Cell Division | Equal divisions | Unequal divisions |
| Duration | 74 days | Years (arrest phases) |
Clinical Significance and Applications
Medical Importance
Understanding gametogenesis is essential for:
- Fertility treatments: IVF, ICSI procedures
- Contraceptive development: Hormonal birth control
- Genetic counseling: Chromosomal abnormalities
- Reproductive health: Diagnosing infertility causes
Research Applications
- Stem cell research: Studying germ cell differentiation
- Cancer research: Understanding testicular and ovarian cancers
- Developmental biology: Embryonic development studies
Study Tips for CBSE Examinations
Important Points to Remember
- Spermatogenesis phases: Memorize the four distinct phases and their outcomes
- Hormonal control: Understand GnRH-LH/FSH-androgen pathway
- Oogenesis timing: Remember meiotic arrest and ovulation timing
- Structural changes: Focus on spermiogenesis transformations
- Comparative aspects: Know differences between male and female gametogenesis
Common Examination Questions
- Describe the phases of spermatogenesis with diagrams
- Explain hormonal control of gametogenesis
- Compare spermatogenesis and oogenesis
- Discuss the significance of meiotic divisions in gamete formation
- Analyze the role of supporting cells (Sertoli and granulosa cells)
Gametogenesis represents one of biology's most remarkable processes, ensuring species continuity through sophisticated cellular differentiation and hormonal regulation. For CBSE students, mastering these concepts provides a strong foundation for understanding reproductive biology, genetics, and developmental processes. The intricate balance between spermatogenesis and oogenesis demonstrates the complexity and elegance of human reproductive systems.
Understanding gametogenesis not only fulfills academic requirements but also provides insights into human health, fertility, and the fundamental processes that govern life itself. This knowledge forms the basis for advanced studies in reproductive medicine, genetics, and biotechnology.