Male Reproductive System: Anatomy, Function, and Physiology
Introduction to Human Reproductive System
The male reproductive system is a complex network of organs and structures designed for the production, maturation, and delivery of male gametes (sperm). Understanding this system is crucial for CBSE Class 12 Biology students as it forms the foundation for topics like human reproduction, genetics, and evolutionary biology.
Classification of Reproductive Organs
Primary Sex Organs (Gonads):
- Testis: Male gonads responsible for sperm production and hormone secretion
- Ovary: Female gonads (for comparison)
- Origin: Mesodermal tissue during embryonic development
Secondary (Accessory) Organs: These structures facilitate transportation, storage, maturation, and fertilization of gametes.
Male Accessory Organs:
- Vasa efferentia
- Vasa deferentia (vas deferens)
- Epididymis
- Seminal vesicles
- Ejaculatory duct
- Prostate gland
- Urethra
- Cowper's glands (bulbourethral glands)
- Penis
Testis: The Primary Male Reproductive Organ
Anatomical Position and Structure
The testis is the primary male gonad, homologous to the female ovary. Each adult testis weighs approximately 10-15 grams and is suspended in the scrotum by the spermatic cord.
Testicular Descent and Temperature Regulation
Extraabdominal Position: Most mammals have extraabdominal testes because spermatogenesis requires a temperature 2-3°C lower than normal body temperature.
Descent Process:
- At birth, testes descend into the scrotal sac
- FSH (Follicle Stimulating Hormone) facilitates this process
- Gubernaculum connects testis to scrotal wall, representing the mesorchium
Exceptions: Some mammals (elephants, sloths, dolphins, whales, sirenians, hyracoidea) have intraabdominal testes.
Seasonal Variation: In seasonal breeders (bats, rats, wolves, foxes), testes descend only during breeding season.
Coverings of the Testis
The testis is protected by three distinct layers:
- Tunica Vaginalis: Outermost covering
- Tunica Albuginea: Fibrous covering beneath tunica vaginalis
- Posterior border forms the mediastinum testis
- Septa divide testis into 200-250 lobules
- Tunica Vasculosa: Innermost vascular coat lining the lobules
Internal Structure of Testis
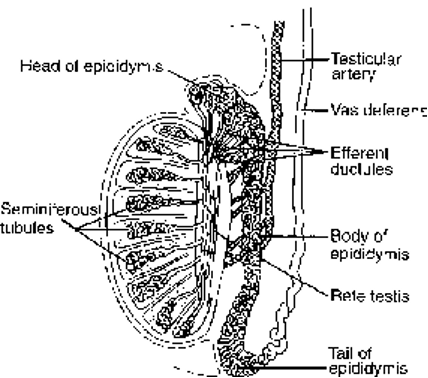
Lobular Organization:
- 200-250 lobules per testis
- Each lobule contains 2-3 seminiferous tubules
- Tubules lined with cells representing various stages of sperm formation
Tubular Network:
- Seminiferous tubules → 20-30 straight tubules (tubuli recti)
- Enter mediastinum → Form rete testis (network)
- 15-20 ciliated efferent ductules (vasa efferentia) emerge from rete testis
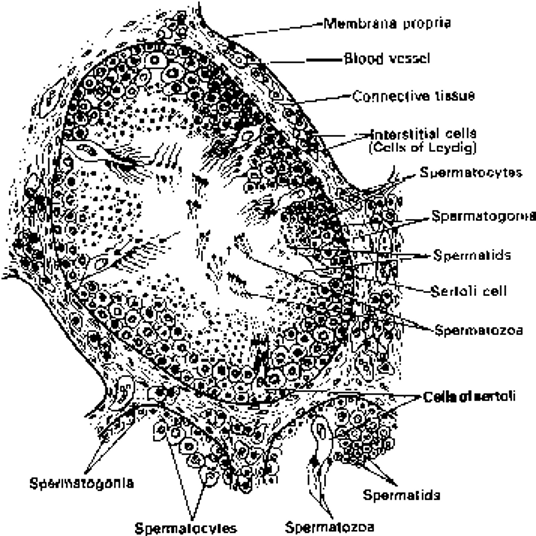
Sertoli Cells: The Nurse Cells
Structure and Function:
- Columnar nutritive cells within seminiferous tubules
- Support developing sperm cells
- Sperm heads embed in Sertoli cells for nutrition
Hormonal Regulation:
- Secrete inhibin hormone
- Inhibin provides negative feedback to FSH synthesis
- Spermiation: Release of mature spermatozoa from Sertoli cells
FSH Dependency: Structure and function maintained by Follicle Stimulating Hormone.
Epididymis: Sperm Maturation Center
Anatomical Structure
The epididymis consists of a single, narrow tube approximately 6 meters long in humans, tightly coiled along the antero-dorsal side of each testis.
Three Distinct Regions:
- Caput epididymis (Head/Globus major)
- Corpus epididymis (Body)
- Cauda epididymis (Tail/Globus minor)
Physiological Functions
Sperm Maturation:
- Storage and activation of spermatozoa
- Sperms acquire motility during epididymal transit
- Contributes secretions to seminal fluid
Storage Capacity:
- Sperms stored primarily in cauda epididymis and vas deferens
- Without ejaculation, sperms are absorbed by epididymal walls
- Human sperm survival: 4 weeks in epididymis
Vas Deferens: The Sperm Highway
Anatomical Course
Structure: 30 cm long straight tube in humans Path: Cauda epididymis → Inguinal canal → Abdominal cavity (with spermatic cord)
Functions
- Secondary storage for mature spermatozoa
- Glandular secretions contribute to seminal fluid
- Vasectomy target: Cut or ligated for birth control
Anatomical Relations:
- Entwines with ureter
- Receives duct from seminal vesicle
- Forms ejaculatory duct
Accessory Glands and Their Secretions
Seminal Vesicles
Location: Between urinary bladder and rectum (approximately 5 cm in humans)
Secretory Products:
- 60-70% of total ejaculate volume
- Fructose: Primary energy source for sperm
- Proteins, citrate, inositol
- Prostaglandins: Facilitate sperm transport
- Sperm possess fructokinase enzyme to metabolize fructose
Species Variation: Rabbits have uterus masculina instead of seminal vesicles.
Prostate Gland
Structure: Chestnut-shaped multilobular gland with 30-40 tubulo-alveolar units
Location: Base of urinary bladder, surrounding prostatic urethra
Secretory Products (30-40% of semen):
- Alkaline fluid (pH regulation)
- Prostaglandins
- Citrate, calcium, phosphate ions
- Clotting enzymes
Clinical Significance:Benign Prostatic Hypertrophy (BPH) in elderly males causes urination difficulties.
Bulbourethral Glands (Cowper's Glands)
Structure: Pair of pea-sized glands at penis base
Functions:
- Secrete viscous alkaline fluid
- Lubrication for copulation
- Neutralizes acidic urine in urethra
- Pre-ejaculatory fluid preparation
Penis: The Copulatory Organ
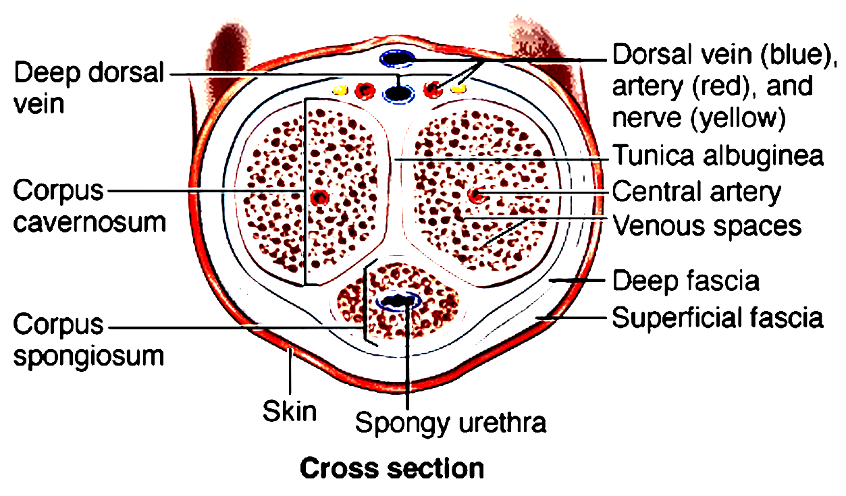
Anatomical Structure
Erectile Tissue Components:
- Corpus cavernosum (paired, dorsal)
- Corpus spongiosum (single, ventral, contains urethra)
External Features:
- Glans penis: Enlarged bulbous tip
- Prepuce (foreskin): Covering of glans
- Glands of Tyson: Secrete smegma (cheese-like substance)
Species Variations:
- Os penis/baculum: Cartilaginous or bony core in rodents, dogs, walrus
- Preputial glands: Equivalent of Tyson's glands in rats
Semen: Composition and Characteristics
Volume and Concentration
Normal Parameters:
- Volume per ejaculation: 3-5 ml
- Sperm concentration: ~100 million per ml
- Oligospermia: <20 million sperm/ml (fertility concerns)
- Azoospermia: Complete absence of sperm
Survival and Function
Sperm Longevity:
- In epididymis: 4 weeks
- In female reproductive tract: 48-72 hours post-ejaculation
Fructose Significance:
- Unique to semen in human body
- Forensic marker for sexual intercourse
Key Biological Parameters and Clinical Conditions
| Parameter | Normal Range | Clinical Significance |
|---|---|---|
| Testis Weight | 10-15 grams | Developmental assessment |
| Testicular Lobules | 200-250 per testis | Spermatogenesis capacity |
| Epididymal Length | ~6 meters | Sperm maturation time |
| Vas Deferens Length | ~30 cm | Surgical considerations |
| Semen Volume | 3-5 ml/ejaculation | Fertility evaluation |
| Sperm Concentration | ~100 million/ml | Fertility assessment |
| Oligospermia Threshold | <20 million/ml | Infertility diagnosis |
| Sperm Survival (Epididymis) | 4 weeks | Storage capacity |
| Sperm Survival (Female tract) | 48-72 hours | Fertilization window |
Hormonal Regulation Summary
| Hormone | Source | Function | Regulation |
|---|---|---|---|
| FSH | Anterior Pituitary | Spermatogenesis support, testicular descent | Inhibited by inhibin |
| Inhibin | Sertoli Cells | FSH negative feedback | Sperm production status |
| Testosterone | Leydig Cells | Secondary sexual characteristics | LH stimulation |
| Prostaglandins | Seminal vesicles, prostate | Sperm transport, smooth muscle contraction | Local regulation |
Clinical Correlations for CBSE Students
Reproductive Health Conditions
Cryptorchidism: Failure of testicular descent
- Cause: FSH deficiency or mechanical obstruction
- Treatment: Hormonal therapy or surgical intervention
Inguinal Hernia: Weakness in inguinal canal
- Risk factor: Spermatic cord passage
- Prevention: Proper lifting techniques
Male Infertility Factors:
- Oligospermia: Low sperm count
- Azoospermia: No sperm production
- Hormonal imbalances: FSH, LH, testosterone deficiencies
Birth Control Methods
Vasectomy:
- Procedure: Cutting or blocking vas deferens
- Effectiveness: >99% when properly performed
- Reversibility: Possible but not guaranteed
Evolutionary and Comparative Aspects
Fertilization Strategies
External Fertilization (Aquatic animals):
- No specialized copulatory organs
- Amplexus in frogs (pseudocopulation)
Internal Fertilization (Terrestrial animals):
- Specialized penis for sperm transfer
- Cloaca-to-cloaca transfer in birds and reptiles
Adaptations Across Species
Temperature Regulation:
- Extraabdominal testes: Most mammals
- Intraabdominal testes: Aquatic mammals, elephants
- Seasonal descent: Hibernating/seasonal breeders
Study Tips for CBSE Examinations
Important Points to Remember
- Testicular descent is FSH-dependent and temperature-related
- Sertoli cells provide both nutrition and hormonal regulation
- Epididymis is crucial for sperm maturation and motility acquisition
- Accessory glands contribute different components to semen
- Hormonal feedback loops maintain reproductive homeostasis
Common Examination Questions
Short Answer Questions:
- Functions of Sertoli cells
- Composition of semen
- Role of accessory glands
Long Answer Questions:
- Complete structure and function of male reproductive system
- Hormonal regulation of male reproduction
- Comparative reproductive strategies
Diagram-Based Questions:
- L.S. of testis with labeling
- Cross-section of penis
- Seminiferous tubule structure
This comprehensive guide provides the essential knowledge required for CBSE Class 12 Biology examinations while maintaining scientific accuracy and educational value. Regular revision of these concepts, along with diagram practice, will ensure thorough preparation for both board examinations and competitive tests.Retry