Hormonal Control of the Female Menstrual Cycle
The reproductive cycle in the female primates (e.g. monkeys, apes and human beings) is called menstrual cycle. The first menstruation begins at puberty and is called menarche. In human females, menstruation is repeated at an average interval of about 28 days, and the cycle of events starting from one menstruation till the next one is called the menstrual cycle.
Do Check - Biotechnology principles
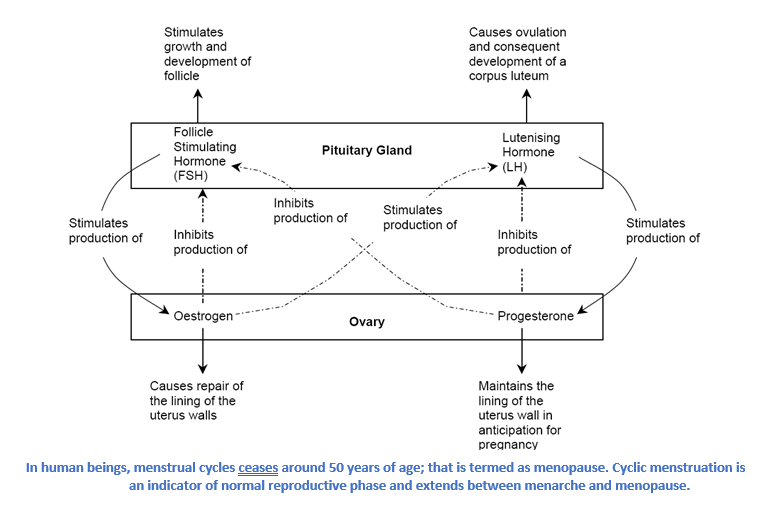
It is controlled by the interaction of several hormones of Hypothalamus, Pituitary and gonadal hormones. The action of one hormone is used to stimulate or inhibit the production of another.
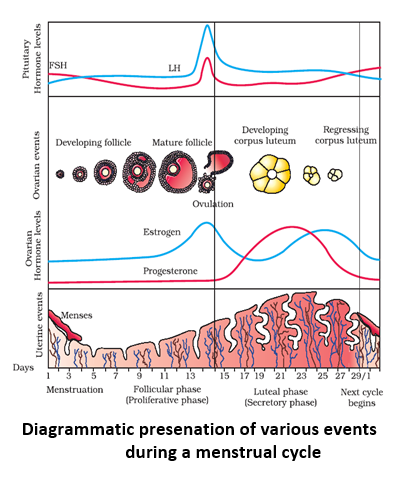
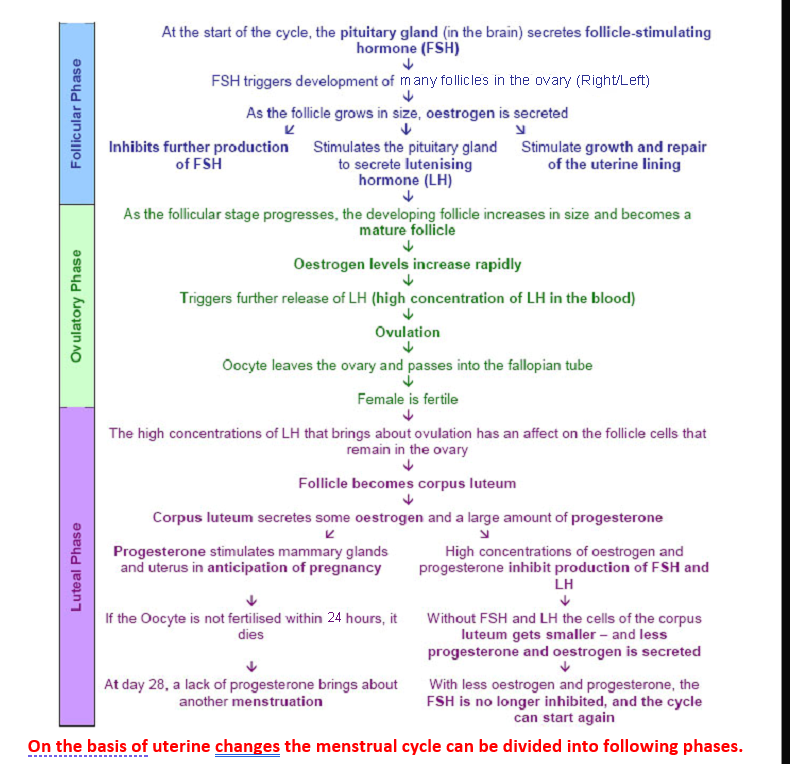
On the basis of ovarian changes the cycle can be divided into three phases: follicular phase, ovulatory phase, and the luteal phase.
- The Follicular phase - is the first part of the menstrual cycle, where one or more follicles start to develop into a mature female gamete. The follicle cells surround the oocyte (developing egg cell), and produce hormones that trigger other responses
- The Ovulatory phase - is when the oocyte is released (follicle cells remain in the ovary) from the ovary and passes down the fallopian tube and towards the uterus
- The Luteal phase - most of the follicle cells remain in the ovary after ovulation. They continue to develop and form a structure called the corpus luteum, as a result more hormones are produced.
- (i) menstrual phase (day 1 – day 3) : Due to falling level of progesterone the uterine wall contracts and extra endometrial lining is shed along with blood and mucus. Volume of blood lost varies from 40 – 150 ml.
- (ii) Proliferative phase (day 3 – day 14) :Uterine endometrium proliferates under influence of estrogen and there is formation of endometrial glands.
- (iii) Secretory phase (day 14 – day 28) : Endometrial glands secrete nutritive substances under influence of progesterone.