According to the World Health Organisation (WHO), reproductive health means a total well-being in all aspects of reproduction, i.e., physical, emotional, behavioural and social. Therefore, a society with people having physically and functionally normal reproductive organs and normal emotional and behavioural interactions among them in all sex-related aspects might be called reproductively healthy
Reproductive Health – Problems and Strategies
India was amongst the first countries in the world to initiate action plans and programmes at a national level to attain total reproductive health as a social goal. These programmes called ‘family planning’were initiated in 1951 and were periodically assessed over the past decades. Improved programmes covering wider reproduction-related areas are currently in operation under the popular name ‘Reproductive and Child Health Care (RCH) programmes’.
- Creating awareness among people about various reproduction related aspects and providing facilities and support for building up a reproductively healthy society are the major tasks under these programmes.
- With the help of audio-visual and the print-media governmental and non-governmental agencies have taken various steps to create awareness among the people about reproduction-related aspects.
- Introduction of sex education in schools should also be encouraged to provide right information to the young so as to discourage children from believing in myths and having misconceptions about sex-related aspects.
- Proper information about reproductive organs, adolescence and related changes, safe and hygienic sexual practices, sexually transmitted diseases (STD), AIDS, etc., would help people, especially those in the adolescent age group to lead a reproductively healthy life.
- Educating people, especially fertile couples and those in marriageable age group, about available birth control options, care of pregnant mothers, post-natal care of the mother and child, importance of breast feeding, equal opportunities for the male and the female child, etc., would address the importance of bringing up socially conscious healthy families of desired size.
- Awareness of problems due to uncontrolled population growth, social evils like sex-abuse and sex-related crimes, etc., need to be created to enable people to think and take up necessary steps to prevent them and thereby build up a socially responsible and healthy society.
Successful implementation of various action plans to attain reproductive health requires strong infrastructural facilities, professional expertise and material support. These are essential to provide medical assistance and care to people in reproduction-related problems like pregnancy, delivery, STDs, abortions, contraception, menstrual problems, infertility, etc. Implementation of better techniques and new strategies from time to time are also required to provide more efficient care and assistance to people. Statutory ban on amniocentesis (a foetal sex determination test based on the chromosomal pattern in the amniotic fluid surrounding the developing embryo) for sex-determination to legally check increasing female foeticides, massive child immunisation, etc., are some programmes that merit mention in this connection.
Also Check: Human Health
Human Population:
Few Terms to Remember
- Human population: The sum total of human beings on earth.
- Demography: The scientific and statistical study of human population. It deals with population growth, its composition (age, sex ratio) and its distribution in space.
- Population density: The number of individuals per square kilometre (km2) at any given time.
- Birth rate (natality): The number of live births per 1000 individuals of population per year.
- Death rate (mortality): The number of deaths per 1000 individuals of population per year.
- Population growth rate: The difference between the birth rate and the death rate.
- Census: The official data of registered number of people in a selected area.
- Total fertility rate (TFR) is the average number of children that would be born to a woman during her lifetime. The total fertility rate varies from region to region.
- Replacement Level (RL) is the number of children a couple must produce to replace themselves so as to maintain the population at zero growth level. RL is slightly higher than 2.0 because some children die before reaching reproductive age. RL is 2.1 in developed countries and 2.7 in developing countries due to a higher death rate at the immature age.
World Population / Indian Population
In the last century an all-round development in various fields significantly improved the quality of life of the people. However, increased health facilities along with better living conditions had an explosive impact on the growth of population. The world population which was around 2 billion (2000 million) in 1900 rocketed to about 6 billions by 2000. A similar trend was observed in India too. Our population which was approximately 350 million at the time of our independence reached close to the billion mark by 2000 and crossed 1 billion in May 2000. That means, every sixth person in the world is an Indian.
Population Growth Rate in India
India is the second most populous country in the world, next to China. India comprises more than 15% of world’s total population. Every population has an inherent tendency to grow. Similarly, the human population is growing. The population of India was about 24 crores in the year 1901. Except for a slight fall in 1911-21, the population of India has been steadily increasing for the last 100 years. As per the census of 2001, as on 1st March 2001, the population of India was 1,027,015,247, i.e. about 102.7 crores. This alarming rate of rise in human population is a cause of concern.
- Density: Indian density of population has increased from 324 people per sq km during Census 2001 to 382 people per sq. km. in 2011 Census. The state of Uttar Pradesh is said to be the most populous state of the Indian Republic and Lakshadweep being least populous.
- Sex Ratio: As per Census 2011, India has got 940 females per every 1000 males. Among all the states and Union Territories of the nation, Pondicherry has got the highest sex ratio of 1038. 2011 Census has reported the lowest child sex ratio of 914 girl children per every 100 boy children.
Factors responsible for population explosion in India
- Advancement in agriculture: With the advancement in the agriculture sector, the availability of food has increased leading to less of starvation and malnutrition.
- Advancement in medicine: With the advancement in medicine, various diseases can be controlled now. This has led to increase in life span. Thus, more and more people live longer, reach reproductive age and produce more children.
- Religious and social customs: Because of prevailing social custom and beliefs many people do not accept family planning measures, leading to rise in population.
- Industrialization: Advancement in industrialization helps in better storage and distribution of food, more employment opportunities and more prosperity.
- Illiteracy: A sizeable number of our population is educated, and yet a large proportion is still illiterate. They are not aware of the functioning of reproductive system and hence the consequence of overpopulation.
- Economic reasons: Children instead of attending school go to work and increase the income of the family.
- Desire for a male child: Even after so much emphasis on gender equity, because of patriarchy in many families, the male child is considered to be essential for continuing the name of the family. The parents want to have at least one son and in this process they give birth to many children sometimes.
A rapid decline in death rate, maternal mortality rate (MMR) and infant mortality rate (IMR) as well as an increase in number of people in reproducible age are probable reasons for this. Through our RCH programmes, though we could bring down the population growth rate, it was only marginal. According to the 2001 census report, the population growth rate was still around 1.7 per cent, i.e., 17/1000/year, a rate at which our population could double in 33 years. Such an alarming growth rate could lead to an absolute scarcity of even the basic requirements, i.e., food, shelter and clothing, in spite of significant progress made in those areas.
Measures to control over population:
- Education: People, particularly those in the reproductive age group, should be educated about the advantage of a small family. Mass media and educational institutions scan play an important role in this campaign. Posters showing a happily married couple with two children with a slogan" Hum Do Humare Do" should be displaced. Many couple even adopted "one child norm".
- Marriageable Age:Raising of the age of marriage is more effective means of controlling the population (now marriageable age of female is 18 years and that of male is 21 years).
- Incentives:Couples with small families should be given incentives.
- Family planning: There are many birth control measures which can check birth rate.
Methods of Contraception:
Contraception is a system or method which knows sexual intercourse but prevents pregnancy.
Although the various contraceptive methods differ in effectiveness and sophistication, the principle of contraception itself is quite simple. As described in a previous section, the process of conception involves the fertilization of an egg by a sperm inside one of the Fallopian tubes leading to the eventual implantation of a growing cell cluster in the uterus, thus starting pregnancy. Obviously then, contraception, or the avoidance of pregnancy, involves an interference with this process by preventing either ovulation, fertilization, or implantation. This interference can take several different forms:
- Preventing the release of an egg from the ovaries ("the pill").
- Preventing the passage of the egg through the Fallopian tube (tubal ligation).
- Preventing the sperm from becoming part of the ejaculated fluid (vasectomy).
- Avoiding coitus at the time when an egg is available for fertilization (rhythm).
- Preventing sperm from being deposited inside the vagina (withdrawal, condom).
- Preventing the sperm inside the vagina from moving through and beyond the cervix (spermicides, diaphragm).
- Hindering the process of implantation (IUD, "morning-after pill").
A wide range of contraceptive methods are presently available which could be broadly grouped into the following categories, namely Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables, Implants and Surgical methods. The method is called temporary method if the effect of the method lasts till the time couple uses the method and fertility resumes immediately after or within few months of its discontinuation.
Natural Methods:
- Abstinence:When the couple refrain from the act of sexual intercourse it is called abstinence. This is 100% successful and has even religious sanction
- Coitus interruptus: It is the oldest method of voluntary fertility control. In this method male withdraws the penis before ejaculation into the vagina and tries to prevent deposition of semen into the vagina or around vulva. This method needs practice and discipline. The failure rate is high.
- Rhythm method: is also known as calendar method or safe period method. This method of contraception depends on the time of ovulation. In a woman having regular menstrual cycle, ovulation occurs on 14th day of the cycle. After ovulation, oocyte remains viable for 24 hours. Similarly, after ejaculation sperms remain alive 72 hours. Thus pregnancy occurs only if coitus is performed during this period. This is the period of high fertility. Therefore, to avoid pregnancy intercourse should be avoided in this period. Rest of the cycle, i.e. 5 – 6 days after bleeding phase of meanstrual cycle and 5–6 days before the next cycle is the safe period (period of least fertility). This method of contraception is successful only if menstrual cycles are regular and woman knows the exact time of ovulation by keeping a record of basal body temperature.
- Lactational amenorrhoea: Lactational amenorrhoea(absence of menstruation) method is based on the fact that ovulation do not occur during the period of intense lactation following parturition due to high level of prolactin. Therefore, as long as the mother breast-feeds the child fully, chances of conception are almost nil. However, this method has been reported to be effective only upto a maximum period of six months following parturition. Chances of failure, though, of this method are also high.
- Barrier Methods: In barrier methods, ovum and sperms are prevented from physically meeting with the help of barriers. Such methods are available for both males and females.
- Male condom made of latex is the most commonly used barrier technique world wide. Modern condoms also contain chemical spermicides. The condom is worn on erect penis before intercourse. ‘Nirodh’ is a popular brand of condom for the male.
- Female condom: made of polyurethane which lines the vagina is also available. Female condoms are about 3 inches wide and 7 inches long, with a flexible ring at each end. Closed end is placed deep in vagina so it covers the cervix (the opening to the uterus). The ring at the open end stays outside the vagina and partly covers the labia (outer genitals).
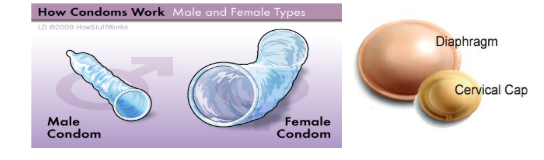
- Diaphragm and cervical cap are other barrier devices applied on the cervix in females. Diaphragm is a rubber sheath with a flexible metal or spring ring at the margin which is fitted inside the vagina. Cervical cap is rubber nipple which is fitted over the cervix and is designed to remain there by suction. The device prevents the entry of sperms into uterus. These are reusable.
Latex male condoms and female condoms are the only birth control methods that prevent HIV and other sexually transmitted diseases, including Chlamydia and gonorrhoea. Spermicidal creams, jellies and foams are usually used along with these barriers to increase their contraceptive efficiency.
Use of condoms has increased in recent years due to its additional benefit of protecting the user from contracting STDs and AIDS. Both the male and the female condoms are disposable, can be self-inserted and thereby gives privacy to the user.
Chemical Method:
(i)Sponge (Today) The contraceptive sponge is a round disposable barrier made of a polyurethane that contains spermicide. Sponge (Today) is a suppository or tablet containing nonoxynol-9 as spermicide. It is placed deep in the vagina and absorbs and traps sperm so that they don't travel up the female genital tract to unite with an egg.
(ii)Spermicide A spermicide is a chemical compound that kills sperm. Nonoxynol-9 is the only spermicide available in Canada. It comes in the form of foam, gel, cream, film or suppository.
Hormonal method:
(i) Combined pills:Combined pills contain a combination of estrogen and progestin. They are categorized as monophasic, biphasic, or triphasic pills depending on whether the level of hormones stays the same during the first three weeks of the menstrual cycle or changes. Combined birth control pills work by preventing ovulation (the release of a mature egg from a woman's ovary). Combined pills thin the endometrium (the lining of the uterus). The hormones also cause the cervical mucus (liquid at the opening of the uterus) to thicken, which can stop sperm from getting into the uterus. The pill also causes changes in the lining of the uterus and the cervical mucus to keep the sperm from joining the egg. Pills have to be taken daily for a period of 21 days starting preferably within the first five days of menstrual cycle. After a gap of 7 days (during which menstruation occurs) it has to be repeated in the same pattern till the female desires to prevent conception. Mala-D is an example of combined pills.
(ii) Progestin-only pills (mini-pills):This type of pills contains no estrogen. Progestin-only pills are ideal for breastfeeding women because estrogen reduces milk production. In addition, progestin-only pills do not have most of the estrogen-related side effects of oral contraception: nausea, headaches and other symptoms associated with starting the combined pill are minimal. However, bleeding and spotting during the intramenstrual period may be higher than with the combined pills and missed pills may result in a higher chance of pregnancy that with the combined oral contraceptives. These pills primarily work by thickening the cervical mucus, thereby preventing sperm from entering the uterus. The minipills do not usually prevent ovulation because they don't contain estrogen. To work effectively, they must be taken at a certain time every 24 hours. Even missing one pill can greatly reduce effectiveness.
(iii) Saheli-The non hormonal contraceptive (Weekly oral contraceptive pill) Central drug Research Institute (CDRI), Lucknow has developed the molecule 'Centchroman' which was marketed by HLL under the brand name Saheli. Introduced in 1991, Saheli has the unique distinction of being the world's first non-steroidaloral contraceptive pills.
It is also unique since it is an indigenously developed drug - the first of its kind. For being non -steroidal, Saheli does not have the short term side effects like nausea, vomiting, weight gain etc. which are commonly reported with the other oral contraceptive pills.
Mechanism of Action: The molecule centchroman offers a unique combination of weak estrogenic and potent anti estrogenic properties. Due to this subtle mix of estrogenic and anti estrogenic action it inhibits the fertilized ovum from nidation (implantation) and thus prevents pregnancy, but at the same time, it does not appear to disturb the other estrogen effects. The contraceptive effect is readily reversible and subsequent pregnancy and its outcome is normal. It scores over steroidal contraceptive pills because it does not disturb the endocrine system and the normal ovulatory cycle is maintained.
Dosage: This pill is to be taken twice a week on fixed days for the first three months, followed by one pill in a week thereafter.
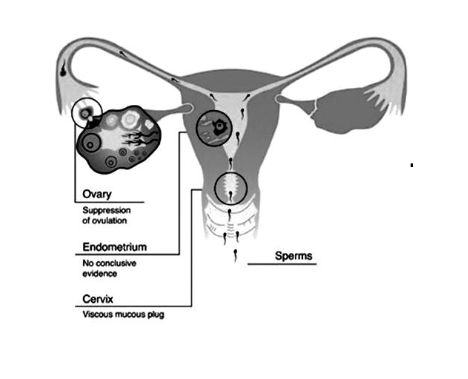
Birth control hormonal pills prevent pregnancy by four ways
(i) Inhibition of ovulation.
(ii) Alternation in uterine endometrium to make it unsuitable for implantation.
(iii) Changes in cervical mucus impairing its ability to allow passage and transport of sperms.
(iv) Inhibition of motility and secretory activity of fallopian tubes.
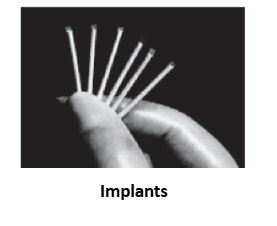
Implants : They are hormone contain devices which are implanted subdermally for providing long term contraception. Norplant is progestin only device. They are inserted under the skin in a fan shaped manner inside upper arm or forearm through a small incision. Norplant remains effective for about 5 years.
Injection: Depo-provera is a single synthetic hormone (Medroxy progesterone acetate + Norethenesterone) that is injected into the muscles of the upper arm. The hormone prevents the release of an egg from the ovaries. It also thickens cervical mucus, which inhibits sperm from moving up the female genital tract.
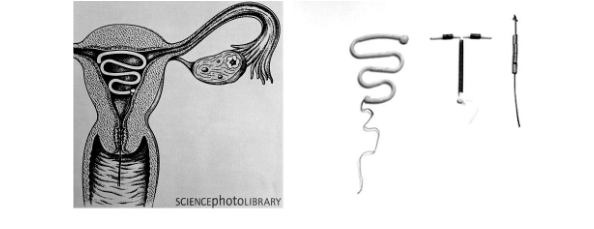
Intrauterine Devices
These devices are inserted by doctors or expert nurses in the uterus through vagina. These Intra Uterine Devices are presently available as the non-medicated IUDs (e.g., Lippes loop), copper releasing IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs (Progestasert, LNG-20).
(i) The hormonal IUD contains a progestin. It prevents pregnancy mainly by thickening the mucus in the cervix making it difficult for sperm to enter the uterus and fertilize the egg. The hormone releasing IUDs, in addition, make the uterus unsuitable for implantation and the cervix hostile to the sperms. IUDs are ideal contraceptives for the females who want to delay pregnancy and/or space children. It is one of most widely accepted methods of contraception in India.
(ii) Copper releasing IUDs increase phagocytosis of sperms within the uterus and the Cu ions released suppress sperm motility and the fertilising capacity of sperms.
Emergency Contraception
Emergency contraception can safely prevent pregnancy after unprotected sexual intercourse. It is useful
(i)When a birth control method fails (for example, if a condom or a diaphragm, breaks or a woman misses several birth control pills.
(ii)When no birth control was used.
(iii)When a woman is a victim of forced sex or rape.
Two methods are available.
(i) Emergency contraception ("morning-after") pills contain hormones. They prevent pregnancy in the same way as birth control pills.
When taken within 72 hours (3 days) after unprotected sex, emergency contraception pills are very effective in preventing pregnancy. The sooner the pills are taken, the more effective they are.
(ii) A copper IUD (intrauterine device) can also be used for emergency contraception.
A copper IUD can prevent pregnancy if inserted by a health care provider within 120 hours (5 days) after unprotected intercourse. It prevents implantation.
Surgical Methods
Also called sterilisation, are generally advised for the male/female partner as a terminal method to prevent any more pregnancies. Surgical intervention blocks gamete transport and thereby prevent conception.
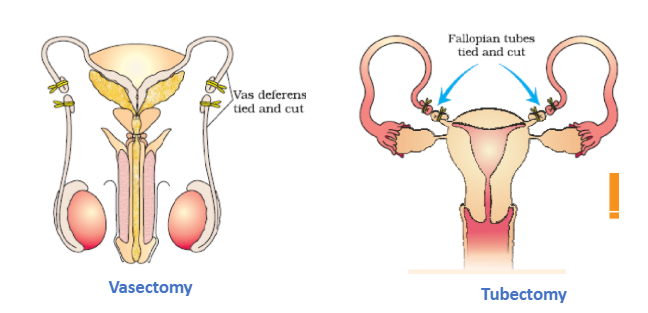
Sterilisation procedure in the male is called ‘vasectomy’ and that in the female, ‘tubectomy’. In vasectomy, a small part of the vas deferens is removed or tied up through a small incision on the scrotum whereas in tubectomy, a small part of the fallopian tube is removed through a small incision in the abdomen or through vagina. These techniques are highly effective but their reversibility is very poor.
However, their possible ill-effects like nausea, abdominal pain, breakthrough bleeding, irregular menstrual bleeding or even breast cancer, though not very significant, should not be totally ignored.
Medical Termination of Pregnancy (MTP)
Intentional or voluntary termination of pregnancy before full term is called medical termination of pregnancy (MTP) or induced abortion. Nearly 45 to 50 million MTPs are performed in a year all over the world which accounts to 1/5th of the total number of conceived pregnancies in a year. Obviously, MTP has a significant role in decreasing the population though it is not meant for that purpose. Whether to accept / legalise MTP or not is being debated upon in many countries due to emotional, ethical, religious and social issues involved in it. Government of India legalised MTP in 1971 with some strict conditions to avoid its misuse. Such restrictions are all the more important to check indiscriminate and illegal female foeticides which are reported to be high in India. Why MTP? Obviously the answer is –to get rid of unwanted pregnancies either due to casual unprotected intercourse or failure of the contraceptive used during coitus or rapes. MTPs are also essential in certain cases where continuation of the pregnancy could be harmful or even fatal either to the mother or to the foetus or both. MTPs are considered relatively safe during the first trimester, i.e., upto 12 weeks of pregnancy. Second trimester abortions are much more riskier. One disturbing trend observed is that a majority of the MTPs are performed illegally by unqualified quacks which are not only unsafe but could be fatal too. Another dangerous trend is the misuse of amniocentesis to determine the sex of the unborn child. Frequently, if the foetus is found to be female, it is followed by MTP- this is totally against what is legal. Such practices should be avoided because these are dangerous both for the young mother and the foetus. Effective counselling on the need to avoid unprotected coitus and the risk factors involved in illegal abortions as well as providing more health care facilities could reverse the mentioned unhealthy trend.
(i) RU-486 (also known as mifepristone) is a synthetic steroid related to progesterone. Unlike the synthetic progestins used in oral contraceptives that mimic the actions of progesterone, RU-486 is a progesterone antagonist; that is, it blocks the action of progesterone. It does this by binding more tightly to the progesterone receptors than progesterone itself but without the normal biological effects:
- The proteins needed to establish and maintain pregnancy are no longer synthesized.
- The endometrium breaks down.
- The embryo detaches from it and can no longer make chorionic gonadotropin (HCG).
- Consequently the corpus luteum ceases its production of progesterone.
- The inhibition on uterine contraction is lifted.
- Soon the embryo and the breakdown products of the endometrium are expelled.
- These properties of RU-486 have caused it to be used to induce abortion of an unwanted foetus. Use of RU-486 is generally limited to the first seven weeks of pregnancy.
(ii) Another option uses the drug methotrexate in combination with misoprostol
- Sexually Transmitted Diseases (STDs): Diseases or infections which are transmitted through sexual intercourse are collectively called sexually transmitted diseases (STD) or venereal diseases (VD) or reproductive tract infections (RTI). Gonorrhoea, syphilis, genital herpes, chlamydiasis, genital warts, trichomoniasis, hepatitis-B and of course, the most discussed infection in the recent years, HIV leading to AIDS are some of the common STDs. Among these, HIV infection is most dangerous.
- Mode of Transmission of STDs : They are caused by germs that live on the skin or in body fluids such as semen, vaginal fluid or blood. The germs are passed from an infected person often through sexual contact with skin, blood or body fluids. These germs can enter the body through the vagina, mouth, anus and open sores or cuts. STDs are not spread by casual contact, by being in swimming pools or by sitting on toilet seats. Some of these infections like hepatitis- B and HIV can also be transmitted by sharing of injection needles, surgical instruments, etc., with infected persons, transfusion of blood, or from an infected mother to the foetus too.
Typical symptoms of STDs :
Early symptoms of most of these are minor and include itching, fluid discharge, slight pain, swelling, etc., in the genital region. Infected females may often be asymptomatic and hence, may remain undetected for long. Absence or less significant symptoms in the early stages of infection and the social stigma attached to the STDs, deter the infected persons from going for timely detection and proper treatment. This could lead to complications latter, which include pelvic inflammatory diseases (PID), abortions, still births, ectopic pregnancies, infertility or even cancer of the reproductive tract.
Brief summary of Some STDs
Chlamydia
Chlamydia trachomatis, or simply chlamydia, is a bacterial infection caused by pathogen (germ) Chlamydia trachomatis that usually infects the genitals of both men and women, but can also infect the throat, rectum and eyes. Chlamydia is one of the most common STD's - and because more than 50% who have chlamydia have no symptoms at all - chlamydia infection usually goes untreated.
-
Chlamydia Symptoms in Women:
- an unusual vaginal discharge
- pain or a burning sensation when passing urine
- bleeding between periods
- pain during sex or bleeding after sex
- low abdominal pain sometimes with nausea
-
Chlamydia Symptoms in Men:
- white/cloudy, watery discharge from the tip of the penis
- pain or a burning sensation when passing urine
- testicular pain and/or swelling
Gonorrhea
It is a bacterial infection caused by Neisseria gonorrheae:
Is a highly contagious sexually transmitted bacterial infection, sometimes referred to as the clap. The nickname of the clap refers to a treatment that was used to clear the blockage in the urethra from gonorrhea pus, where the penis would be 'clapped' on both sides simultaneously. This gonorrhea treatment is rarely used today, however the nomenclature remains. Gonorrhea is characterized by thick discharge from the penis or vagina. In addition to male reproductive organs & female genital tract, gonorrhea may infect the rectum, throat, eyes, blood, skin, & joints.
-
Gonorrhea Symptoms in Women
- Strong smelling vaginal discharge that may be thin & watery or thick & yellow/green
- Irritation or discharge from the anus
- Abnormal vaginal bleeding
- Possibly some low abdominal or pelvic tenderness
- Pain or a burning sensation when passing urine
- Low abdominal pain sometimes with nausea
-
Gonorrhea Symptoms in Men
- White, yellow or green thick discharge from the tip of the penis
- Inflammation of the testicles & prostate gland
- Irritation or discharge from the anus
- Urethral itch & pain or burning sensation when passing urine
Hepatitis:
- There are five types of hepatitis -- A to E -- all of which cause inflammation of the liver. Type D affects only those who also have hepatitis B, and hepatitis E is extremely rare.
- Type Ahepatitis is contracted through anal-oral contact, by coming in contact with the feces of someone with hepatitis A, or by eating or drinking hepatitis A contaminated food or water.
- Type Bhepatitis can be contracted from infected blood, seminal fluid, vaginal secretions, or contaminated drug needles, including tattoo or body-piercing equipment. It can also be spread from a mother to her baby.
- Type Chepatitis is not easily spread through sex. You're more likely to get it through contact with infected blood, contaminated razors, needles, tattoo and body-piercing equipment, or manicure or pedicure tools that haven't been properly sanitized, and a mother can pass it to her baby during delivery.
- Type Dhepatitis can be passed through contact with infected blood, contaminated needles, or by sexual contact with an HIV-infected person.
- Type Ehepatitis is most likely to be transmitted in feces, through oral contact, or in water that's been contaminated.
- Symptoms: When symptoms are present, they are much the same for all five types of hepatitis: mild flu-like symptoms, light stools, dark urine, jaundice (yellowing of the skin and the whites of the eyes), fatigue, and fever. Hepatitis A symptoms may also include nausea, vomiting, and abdominal pain.
Herpes
- Both herpes simplex virus-1 and virus-2 may be transmitted through sex, or by kissing or touching any affected area. A condom can prevent herpes transmission during vaginal or anal sex, but oral contact with genitals or open sores anywhere can spread the disease. Washing hands can also minimize transmission.
- Symptoms: Herpes simplex virus-1 usually shows up as cold sores or blisters. For those who have herpes simplex virus-2, some have no symptoms, while others may show signs of an infection from five to twenty days after having sex with an infected partner. Early symptoms can include a burning sensation in the genitals, low back pain, pain when urinating, and flu-like symptoms. A short while later, small red bumps may appear around the genitals or on the mouth; later these bumps become painful blisters which then crust over, form a scab, and heal.
HIV / AIDS
- HIV is the acronym for the Human Immunodeficiency Virus, a virus that attacks the body's immune system, leading to full-blown AIDS (Acquired Immunodeficiency Syndrome). AIDS is devastating because it leaves the body susceptible to life-threatening infections and certain kinds of cancers.
- Symptoms: Most symptoms of AIDS are not caused directly by HIV, but by an infection or other condition brought on by a weakened immune system. These include severe weight loss, fever, headache, night sweats, fatigue, severe diarrhea, shortness of breath, and difficulty in swallowing. The symptoms tend to last for weeks or months at a time and do not go away without treatment. In some cases, infections result in death.
Syphilis
- A bacterial (Treponema pallidum)infection caused by an organism called a spirochete.
- Symptoms: During the first stage of syphilis infection, painless sores or open ulcers may appear on the anus, vagina, penis, or inside the mouth, and occasionally on other parts of the body. During the second stage (roughly three weeks to three months after the first symptoms appear), an infected person may experience flu-like symptoms and possibly hair loss or a rash on the soles and palms -- and in some cases all over the body. There are also latent phases of syphilis infection during which symptoms are absent.
Trichomoniasis
Trichomoniasis, (also called "trich") is a common sexually transmitted disease (STD) that affects both men and women. Trichomoniasis is caused by a protozoan parasite called Trichomonas vaginalis and is a cause of vaginal infections in women and urethral infections in men. Trichomoniasis is one of the most common, (curable) vaginal infection in women.
Trichomoniasis Symptoms in Women
- Genital itching and/or burning
- Vaginal or vulval redness
- Frothy yellow-green vaginal discharge with a strong odor
- Blood spotting
- Frequent and/or painful urination
- Discomfort during intercourse
- Abdominal pain
A woman might also find that the above symptoms worsen after menstruation and that the symptoms may be confused with an yeast infection. This fact emphasizes the importance of always having an yeast infection diagnosed properly, because it might not be an yeast infection.
Trichomoniasis Symptoms in Men
Men are usually asymptomatic, but if a man has symptoms, they can include:
- Unusual penile discharge
- Painful urination
- Burning sensation after ejaculation
- Tingling inside the penis
Crabs or Pubic Lice
Crabs or pubic lice are small crab-shaped parasites that burrow into the skin to feed on blood. They live on coarse body hair, predominantly pubic hair, but can also be found in armpit hair, facial hair and even on eyelashes. The lice are yellow-grey in colour and use their crab-like claws to grip hair strands. They can sometimes be spotted moving on the skin.
Crabs are easily passed on during sex, but can also be passed on through sharing clothes, towels or bedding with someone who has them. Crabs cannot be transmitted via toilet seats or swimming pools.
Symptoms of crabs are usually noticed around 5 days to 7 weeks after infection and include:
- Itchy skin;
- Inflammation of the affected area;
- Sometimes visible lice and eggs;
- Spots of blood as lice feed from blood vessels in the skin.
Genital warts
Genital warts are caused by some sub-types of human papilloma virus (HPV). They can appear on the skin anywhere in the genital area as small whitish or flesh-coloured bumps, or larger, fleshy, cauliflower-like lumps. They are unlikely to cause pain but may itch and can be difficult to spot. Often there are no other symptoms of genital warts, but if a woman has a wart on her cervix she may experience slight bleeding or unusual coloured vaginal discharge.
Thrush
Thrush, also known as candidiasis, is a yeast infection caused by the Candida species of fungus. Thrush is not technically a sexually transmitted infection, as Candida is a common yeast that is found on the skin and genitals of most people, even those who have not had sex. Candida is usually suppressed by the immune system and the natural bacteria found in the body, but there are many things that can upset the balance and allow Candida to grow. Thrush occurs a lot less frequently in men.
The symptoms of a thrush infection are:
- In women - irritation, itching, thick white discharge, redness, soreness and swelling of the vagina and vulva.
- In men - irritation, discharge from the penis, difficulty pulling back the foreskin usually caused by the swelling of the head of the penis (balanitis).
Preventition of STD’s
Except for hepatitis-B, genital herpes and HIV infections, other diseases are completely curable if detected early and treated properly. STDs are a major threat to a healthy society. Therefore, prevention or early detection and cure of these diseases are given prime consideration under the reproductive health-care programmes. Though all persons are vulnerable to these infections, their incidences are reported to be very high among persons in the age group of 15-24 years. We can be free of these infections if we follow the simple principles given below:
(i)Avoid sex with unknown partners/multiple partners.
(ii)Always use condoms during coitus.
(iii)In case of doubt, go to a qualified doctor for early detection and get complete treatment if diagnosed with disease.
Infertility
A discussion on reproductive health is incomplete without a mention of infertility. A large number of couples all over the world including India are infertile, i.e., they are unable to produce children inspite of unprotected sexual co-habitation. The reasons for this could be many–physical, congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but more often than not, the problem lies in the male partner. Specialised health care units (infertility clinics, etc.) could help in diagnosis and corrective treatment of some of these disorders and enable these couples to have children. However, where such corrections are not possible, the couples could be assisted to have children through certain special techniques commonly known as assisted reproductive technologies (ART).
Test-Tube Babies (IVF)-
- They can be developed by, or for those women, who are unable to have normal conception.
- The mature gametes of such women are taken out from ovary and are fertilized in test-tube (in vitro) with their husband’s sperms or with the ‘sperm’ borrowed from sperm bank.
- Such fertilized eggs are allowed to develop, in vitro, upto 32-celled stage (blastocyst), and then the embryo is implanted in the uterus of the same woman or a gestational or surrogate (hired) mother.
- 1st test-tube or IVF (In vitro fertilization) baby, named Louise Joy Brown, was born on July 25th, 1978 in England, by the method developed by 3-scientists, i.e. Dr. Steptoe, Edward and Bavister.
ZIFT-
- Zygote intrafallopian transfer (ZIFT) is another variation of IVF, and is also called as ‘tubal embryo transfer’. In this case after in vitro fertilization (in petridish or test tube) the zygote or early embryo with upto 8 blastomeres is transferred into fallopian tube. Embryos with more than 8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete its further development. Embryos formed by in-vivo fertilisation (fusion of gametes within the female) also could be used for such transfer to assist those females who cannot conceive.
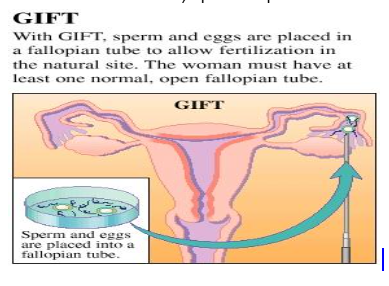
GIFT
GIFT is an assisted reproductive technology procedure in which the eggs are removed, combined with the sperm and then placed inside of the fallopian tubes for fertilization.
This infertility treatment procedure differs from IVF, because in IVF, fertilization occurs in the lab as opposed to in the fallopian tubes.
|
The following steps are involved in a typical gamete intrafallopian transfer procedure:
Because it uses an extra surgical procedure - a laparoscopy - GIFT is considered a more invasive process than IVF. |
GIFT :With GIFT, sperm and eggs are placed in a fallopian tube to allow fertilization in the natural site. The woman must have at least one normal, open fallopian tube. |
- The difference in ZIFT and GIFT is that in ZIFT the fertilization is observed/assured, whereas in GIFT it is not.
- The success rate of IVF/GIFT/ZIFT declines with the advancement of the age of the woman, perhaps due to poor quality of eggs; and if success rate is improved, the chances of multiple births are increased.
ICSI
Intra cytoplasmic sperm injection (ICSI) is another specialised procedure to form an embryo in the laboratory in which a sperm is directly injected into the ovum.
AI
Infertility cases either due to inability of the male partner to inseminate the female or due to very low sperm counts in the ejaculates, could be corrected by artificial insemination (AI) technique. In this technique, the semen collected either from the husband or a healthy donor is artificially introduced either into the vagina or into the uterus (IUI – intra-uterine insemination) of the female.
Though options are many, all these techniques require extremely high precision handling by specialised professionals and expensive instrumentation. Therefore, these facilities are presently available only in very few centres in the country. Obviously their benefits are affordable to only a limited number of people. Emotional, religious and social factors are also deterrents in the adoption of these methods. Since the ultimate aim of all these procedures is to have children, in India we have so many orphaned and destitute children, who would probably not survive till maturity, unless taken care of. Our laws permit legal adoption and it is as yet, one of the best methods for couples looking for parenthood.
Summary of the chapter
∙Reproductive health means a total well being in all aspects of reproduction ie physical, emotional, behavioural and social.
∙India is the first country in the world to initiate action plans and programmes such as Family planning' at the national level to attain total reproductive health
∙Reproductive and Child Health Care (RCH) programmes create awareness among people about reproduction related problems and providing facilities and support for building up a reproductively healthy society.
∙Introduction of sex education in schools be encouraged to provide right information to young ones so as to discourage children from believing in myths and having misconception about sex-related aspects such as proper information about reproductive organs, adolescence and related changes, safe and hygienic sexual practices, sexually transmitted diseases etc.
∙Educating people about the problems due to uncontrolled population growth, social evils like sex-abuse and sex related crimes to build up a socially responsible and healthy society.
∙Increased health facilities along with better living conditions have resulted in population explosion.
∙Our population has crossed I billion in May 2000. Rapid decline in death rate
(a)Maternal mortality rate (MMR),
(b)Infant mortality rate (IMR), and increase in the number of people in reproductive age are the two main reasons for increased population growth in India, a rate at which our population could double in 33 years.
∙There is absolute scarcity in the basic requirement, e.g., food, shelter, water and clothing etc. inspite of significant progress made in those area.
∙Motivation for smaller families by using various contraceptive methods, is the most important step to solve this problem.
∙Natural methods include avoiding chances of ovum and sperms meeting. It include
(a)Periodic abstinence
(b)Withdrawl or Coitus interruptus
(c)Lactational amenorrhea-absence of menstruation cycle during the period of intense lactation following child birth/parturition.
∙Barrier methods include
(a)Condom-Nirodh is a condom for male, vagina and cervix condom for female. also protect the user form contracting STDs and AIDs
(b)Diaphragm, cervical caps and vaults are barriers made up of rubber, inserted in the female to cover cervix during coitus,
(c)Chemicals barriers include spermicidal creams, jellies and foams, used to increase contraceptive efficiency.
Intra-uterine Devices (IUDs):
(i)They are inserted in the uterus by doctors or expert nurses, non-medicated e.g. lippers loop, copper releasing IUDs (Cu-T, Cu7, multiload 375)
(ii)Hormone releasing lUD's (Progestasert, LNG-20). Cu ions suppress sperm motility while hormones make uterus unsuitable for implantation. IUDs ideal for female to delay pregnancy or space children.
∙Oral pills (Progestrone or progestron and estrogen) inhibit ovulation and implantation. "Saheli", a new oral pill is used "once-a-week", a steroid preparation with very less side effects and high contraceptive value.
∙Surgical methods: It includes
(i)Vasectomy - cutting and ligating vas deferens in males
(ii)Tubectomy - cutting and ligating fallopian tubes in females.
∙Medical termination of pregnancy: MTP involve intentional or voluntary termination of pregnancy before full term. It has significant role in decreasing population. It is safe during the first trimester of pregnancy.
∙Sexually transmitted disease: Gonorrhea, syphilis, chlamydia, genetical herpes, hepatitis-B genital warts, HIV-leading to AIDs are some of the diseases or infections transmitted through sexual intercourse and are termed assexually transmitted diseases(STDs).
∙Transmission of STDs: STDs are transmitted through sharing of needles and surgical instruments with infected persons transfusion of blood, or from an infected mother to her baby.
∙Hepatitis-B, genital herpes and HIV-infections are incurable.
∙Symptoms of STDs: It include itching, fluid discharge, slight pain, swellings etc in early stage leading to complications such as pelvic inflammatory diseases (PID) abortions, still birth, ectopic pregnancies, infertility or even cancer of reproductive tract if not detected and properly treated timely.
∙Prevention ofSTDs: STDs are a major threat to healthy society. It can be prevented by
(i)avoiding sex with unknown/multiple partners.
(ii)always use condoms during sexual intercourse,
(iii)in case of doubt, go to a qualified doctor for early detection and complete treatment
∙Infertility: The inability to produce children inspite of unprotected sexual co-habitation for atleast two years is called infertility.
∙Causes:Physical, congenital diseases, drugs, immunological or even physiological reasons cause infertility.
∙Specialised health care units, infertility clinics etc. help in diagnosis and corrective treatment of disorders causing infertility.
∙Test-tube baby programme includein-vitro fertilisation of egg (IVF) followed by embryo transfer (ET) is one of such method
(i)Embryo transfer at 8-celled blastomere stage in fallopian tube of female is called zygote intra-fallopian transfer (ZIFT) or
(ii)Embryos with 16, or 32 blastomere stage are transferred into the uterus to complete further development and termed asIntrauterine transfer (IUT)
∙In vivo fertilisation involve the transfer of embryo from a female to another female who cannot conceive.
∙Gamete intra fallopian transfer: It include the transfer of an ovum from a donor into the fallopian tube of another female who cannot ovulate due to one or other reason.
∙Intra-cytoplasmic Sperm injection (ICSI). It is a method to form an embryo in the laboratory in which the sperm is directly injected into ovum.
∙Artificial insemination (AI) – It involve the introduction of the semen collected from husband / healthy donor into the vagina or into the uterus (IU) – Intra uterine insemination) of the female.
∙Adoption-The best method to overcome the problems of infertility for the middle class couples looking for parenthood is to adopt orphan and destitute children who would probably not survive till maturity, unless taken care of.
Some Important Terms
- Reproductive Health: Refers to a total well being in physical, emotional, behavioural and social aspects of reproduction.
- Amniocentesis: A foetal sex determination test based on chromosomal pattern in the amniotic fluid surrounding the developing embryo.
- Population explosion: An enormous increase in the size of a population in a short span of time.
- Periodic abstinence: Avoiding or abstaining from sex from 10-17 day of the menstrual cycle, when ovulation could be expected.
- Lactational amenorrhea: Absence of menstruation and ovulation during the period of intense lactation following parturition.
- Coitus interruptus: Withdrawl of penis from the vagina just before ejaculation to avoid insemination.
- Sterilisation: Inability to produce sex-cells.
- Vasectomy: Cutting and ligating vas deferens, to prevent sperm transport and thereby prevent conception.
- Tubectomy: Cutting and ligating fallopian tubes to prevent transport of eggs. Hence, sperms transport to fallopian tube is prevented.
- STDs: Diseases or infections transmitted through sexual intercourse.
- Infertility: Inability to produce children inspite of unprotected sexual co-habitation.
- In vitro fertilisation: Refers to the fusion of gametes, outside the body of the female in almost similar conditions as that of the body in the laboratory.
- Artificial insemination: Semen collected either from the husband or a healthy donor is artifically introduced in the vagina or into the uterus of the female.
- Intra-uterine devices (IUDs)-Devices inserted in the uterus through vagina to achieve contraception.
Medical termination of pregnancy (MTP): Intentional or voluntary termination of pregnancy before full term.